Study findings a ‘game-changer’ for treatment of a collapsed lung
A landmark study on the best treatment for patients suffering from a collapsed lung, or pneumothorax, has found that the traditional ‘interventional approach’ of treating the condition with a chest tube is not always in the patient’s best interest.
The six year study, involving more than 300 patients, found that patients who were treated with a ‘conservative’ approach of simple pain relief, observation and awaiting the lung to naturally re-expand and recover, were less likely to have complications and had shorter hospital stays than those who were given a chest tube.
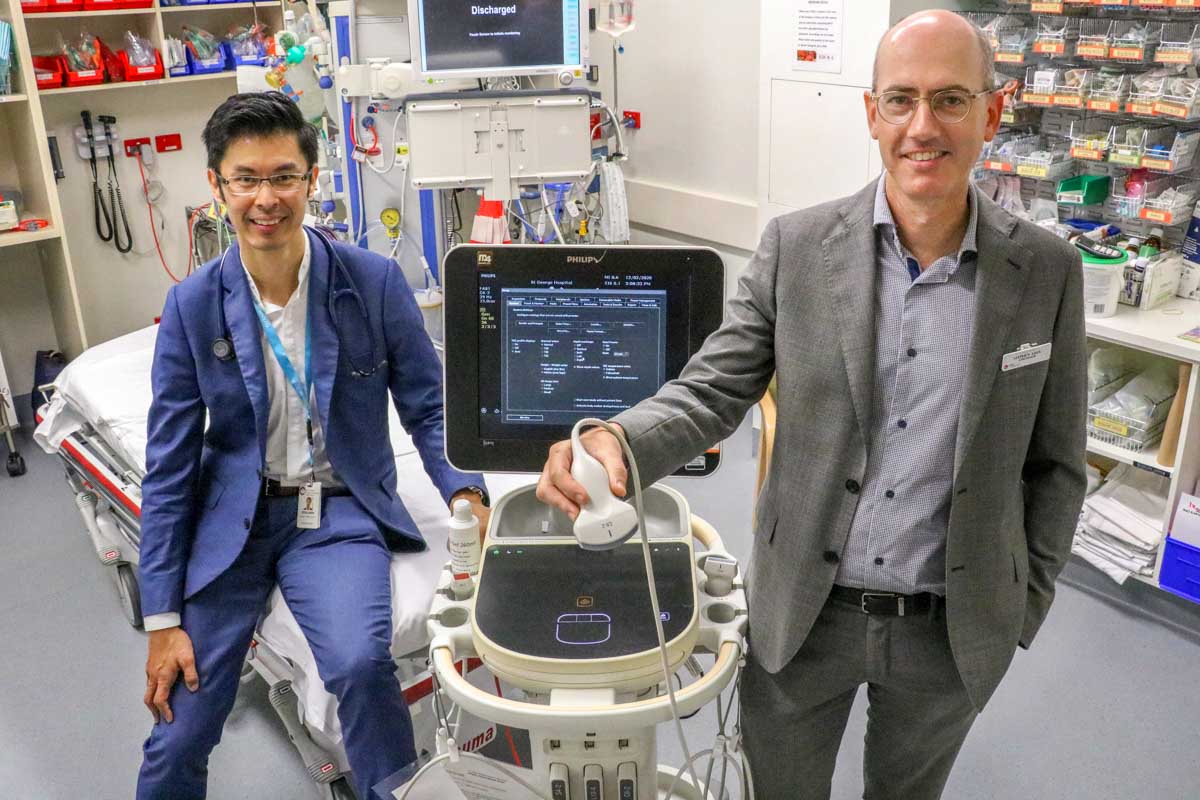
The research was conducted as a collaboration between Australian and New Zealand researchers, including Dr Ben Kwan, Dr David Mah, Dr Allison Moore from The Sutherland Hospital and Dr Stephen Asha and Dr Steven Lindstrom from St George Hospital and many junior medical officers and UNSW students from the emergency departments and respiratory medicine wards across both hospitals.
Clinical researcher Dr Ben Kwan said being a part of the study and a member of the Steering Committee was a rewarding journey.
“It was exciting to work with a large group of colleagues and learn from each other while challenging some of our pre-existing conceptions in regards to treatment outcomes,” Dr Kwan said.
“It was fantastic to see how the respiratory and emergency departments across both sites worked collaboratively in this unique study that has challenged our assumptions that intervention in patients with primary spontaneous pneumothorax is always needed.
“To better inform and educate our patients in regards to the pros and cons of intervention, we need to know how safe and effective it is to do the contrary, i.e. adopt a conservative approach. With this result, we can now adopt a much more personalised approach, and carefully select those patients who may be suitable for conservative treatment, and those where interventions are needed.”
Dr Stephen Asha was the principal investigator at St George Hospital, a member of the Steering Committee and one of the study authors.
“The results suggest that for the majority of patients we can avoid an invasive procedure that is painful and unpleasant, and occasionally can have serious complications,” Dr Asha said.
“These are very important results that should be practice-changing and lead to a big improvement in patient care. I’d like to acknowledge the nurses and doctors in the emergency department for their enthusiasm in helping identify and recruit patients into the study and support the successful conduct of this research.”
The findings were recently published in the prestigious New England Journal of Medicine (NEJM).