Sutherland Supportive and Palliative Care Service
The Supportive and Palliative Care Service at The Sutherland Hospital aims at improving the quality of life of patients with any life-limiting illness, not just cancer. Palliative Care is not just about caring for patients who are dying. We endeavour to provide support by improving pain and other physical symptoms, attending to psychosocial needs and ensuring patients have the information they need to help plan for their ongoing care in the context of their values and wishes.
The Cardiac and Respiratory Supportive Care clinics are able to review patients at home if required. Our other clinics (Palliative Care and Supportive Care Multi-Disciplinary Team) require patients to physically attend our clinic for at least their initial review following which we can provide in-person or telehealth follow-up (we are unable to provide home visits for these clinics).
Please note the Renal Supportive Care Clinic is run separately to the Supportive and Palliative Care Clinics listed here. Referral forms can be found on the St George Renal Service website.
The Palliative Care team consists of Palliative Care Staff Specialists (listed below) and Specialised Nurses. Our Supportive Care Multi-Disciplinary Team (MDT) Clinic includes Social Work, Occupational Therapy, Physiotherapy, Dietitian and Speech Pathology.
Dr Camilla Chan (Monday – Thursday): TSH inpatient consults, Palliative Care Clinic and Supportive Care MDT Clinic
Dr Johnathan Man (Tuesday and Thursday): TSH inpatient consults, Respiratory Supportive Care
Dr Jessica Jones (Monday, Wednesday and Friday): TSH inpatient consults, Palliative Care Clinic, Cardiac Supportive Care"
- Must be over 18 years of age
- Must have a diagnosis of a life-limiting illness
- Must live within the Sutherland area
- Must have at least one of the following general triggers:
- Complex and increasing symptom burden
- Persistent symptoms, despite optimal treatment of underlying condition(s)
- Deterioration in functional performance status and increased support needs
- Patient requires advance care planning
- Progressive weight loss of more than 10% dry body mass, in last 6 months
- Two or more unplanned acute admissions in the last 12 months
- Patient or family requesting supportive and/or palliative care input
Please note: Patients who are rapidly deteriorating and felt to be in the last 3 months of life would be more appropriately referred to the Calvary Community Palliative Care Team
The process for referring a patient is:
1. GP/referrer to send through referral with medication list, relevant imaging, pathology and valid provider number via email or fax:
- SESLHD-TSH-Outpatients@health.nsw.gov.au
- Fax: 9540 8067.
2. Please indicate on the referral which clinic you are referring to:
- Palliative Care
- Supportive Care MDT
- Respiratory Supportive Care
- Cardiac Supportive Care
3. The referral will be checked to ensure it is valid, if not extra information will be sourced from the referrer
4. If valid the referral will be triaged by a Palliative Care Specialist or Care Co-ordinator Nurse
5. Appointment made as per triage recommendation
6 . Patient notified by phone call as well as a text reminder 2 days prior to the appointment
If you wish to discuss which clinic would be the most appropriate for your patient or if your patient requires urgent review, please contact our nurse care co-ordinator on 0417 946 791.
Yes. All referrals are prioritised and allocated according to clinical urgency. Please contact our Nurse Care Co-ordinator if your patient requires urgent review on 0417 946 791.
If you feel you or your loved one would benefit from our service, please discuss with your GP or specialist and request that they send us a referral letter together with all relevant test results.
Once we have received a completed referral, you will be contacted regarding your appointment and receive a text reminder 2 days prior to your appointment.
If you need to change or cancel your appointment, please call us on 9540 8453
On the day of your appointment, please bring:
- Current Medicare card or Veteran Affairs card.
- Any Health Care Card, Pensioner Concession Card or Commonwealth Seniors Health Care Card.
- Insurer details (eg workers compensation, public liability or third party).
- Your Private Health Fund Membership card if you are currently insured with a private health fund.
- A list of your current medications
Please let us know if you need an interpreter. You can contact us by telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak, and then ask the interpreter to set up a telephone conversation between you, an interpreter, and us on 9540 8453.
If you hold a valid Medicare card the visit is Bulk Billed with no gap payment.
If you do not hold a Medicare card, please contact the clinic for further information on fees and payment.
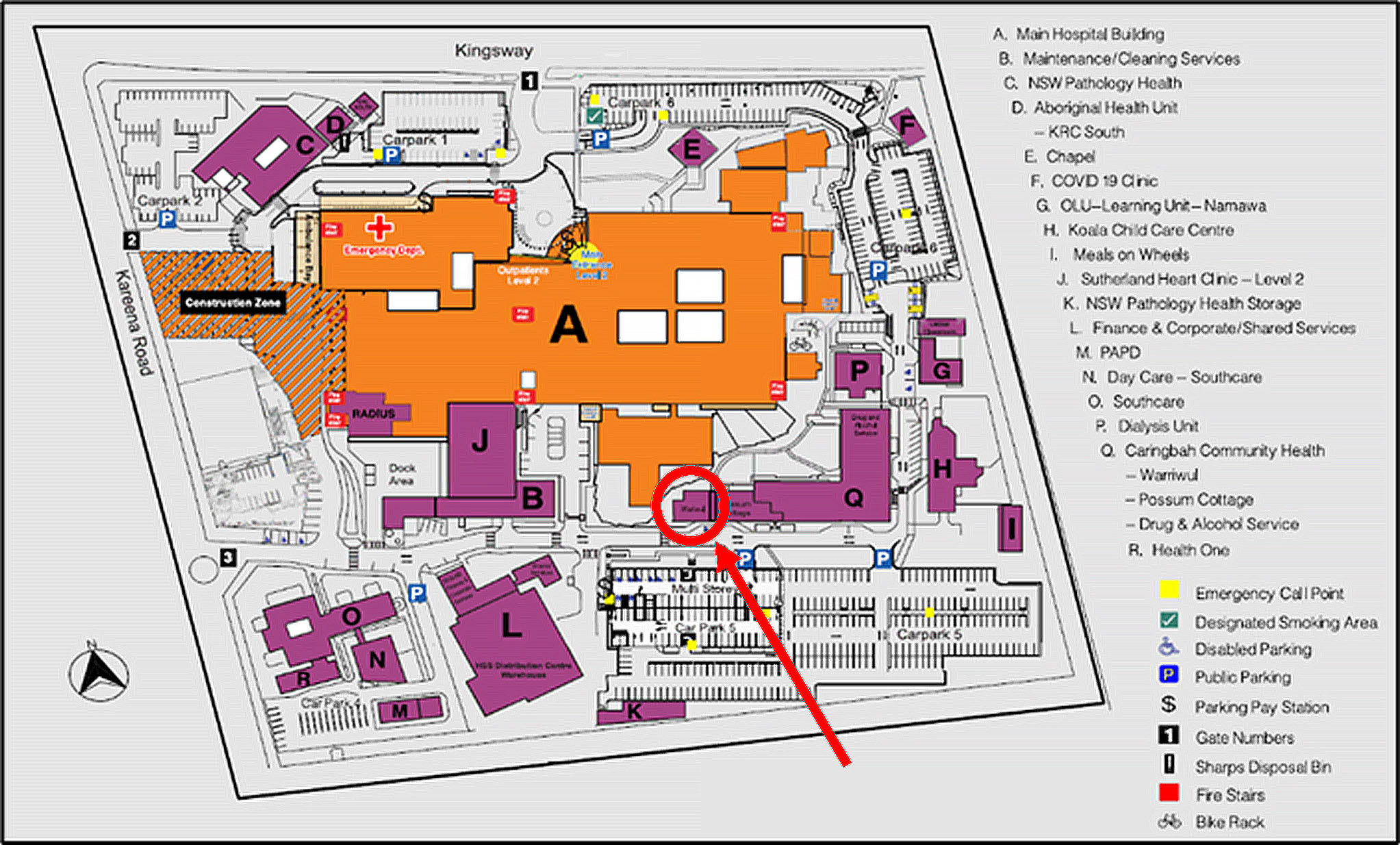
We are located in the Warriwul building on the grounds of Sutherland Hospital, opposite the multi-storey car park. See hospital site map below. Opposite Possum Cottage in the area marked.