Aboriginal Hospital Liaison Service

How we can help you
We acknowledge Prince of Wales Hospital is on land traditionally owned by the Bidjigal/Bidiagal people. We pay our respects to Elders past and present and all Aboriginal and Torres Strait Islander people using our services.
We welcome all people requiring care and their families, carers and friends to our hospital.
We ask all people coming to our hospital ‘Are you living as or known as an Aboriginal or Torres Strait Islander in your community?’ If you answer yes, we will ask you if you would like to see our Aboriginal Hospital Liaison Officers (AHLOs).
Coming to hospital can be a difficult time. Our AHLOs are available to have a yarn if you are finding it difficult being away from your home and family, if you are dealing with Sorry Business or feel a bit lonely or anxious.
Our AHLOs are part of our Social Work team and available to provide you the following support:
- Provide you with and your family with emotional, social and cultural support
- Advocate and liaise with other staff on your behalf
- Provide information about hospital services
- Provide information on your rights and responsibilities
- Organise referrals to other services (eg Aboriginal, Legal, Child Care Protection)
- Help you get financial assistance if you need it (eg pensions, benefits, IPTAAS (Isolated Patient’s Travel and Accommodation Scheme))
- Help you with finding accommodation if you are travelling to Sydney from the country
- Help you to fill in an application for housing
- Organise nursing, hospice or respite care if you need it
- Organise for you to get help if you need it when you get home. This includes help with housework, shopping, meals on wheels or any equipment you might need.
You can read our brochure for more information.
Aboriginal Hospital Liaison Officers
Aunty Linda Boney linda.boney@health.nsw.gov.au
Jeremy Davison jeremy.davison@health.nsw.gov.au
Charlee Lester charlee.lester@health.nsw.gov.au
If you cannot contact Aunty Linda or Jeremy on the direct telephone numbers above, call the switchboard on 9382 2222 and dial 0 to speak with someone. Ask them to page an Aboriginal Hospital Liaison Officer.
How to find us
Social Work Department, Level 3, High Street Building, Prince of Wales Hospital (Building 2 on our campus map)
Information about how to get to our Randwick campus
Barmbli Place is a room where Aboriginal and Torres Strait Islander people can come for a cuppa, yarn or just sit while a family member is in hospital.
Barmbli Place is at the High St entrance of Prince of Wales Hospital. It is open from 8am to 8pm, seven days a week. If you need help to find us please ask the person at the High St information desk.

Pain Management Department
How we can help you
We help you manage your pain and its impact on your life. We focus on the medical, physical, social, psychological and environmental factors associated with pain.
We can help you develop a plan to:
- reduce how much pain you are feeling
- increase what you can do
- regain control of your life, and
- improve the quality of your life.
Managers
Director A/Prof K E Khor
Nurse Manager David Begley
Opening hours
Pain Clinic days are Monday, Tuesday, Wednesday & Friday.
Learn about our electronic referral system
How to find us
The Prince of Wales Hospital Pain Management Services (and Pain Clinic) are located at: Outpatients Department, Level 2, Campus Centre, Prince of Wales Hospital (Building 16 on our campus map)
Information about how to get to our Randwick campus
We are a team of health professionals, based in the hospital, who will work with you to help you manage your pain.
Our doctors specialise in pain medicine, anaesthesia, geriatric medicine, addiction medicine, psychiatry and rehabilitation medicine. They will help you:
- Understand your pain and what may be causing it
- Reduce your pain using medicines and other treatments
- Maximise what you are able to do when you have pain
- Understand how your pain is affecting your physical and emotional health
- Use prescribed pain medicines safely
- Manage short term experiences of acute pain such as after having surgery.
Our nurses will assess your pain, give you education and pain treatments. Our nurses can help answer questions you have about treatments or medicines. Our nurses also will work with you in our pain programs, focusing on mindfulness and medicines.
Our physiotherapist will have time to explain what is happening when your body is in pain and how that can impact how you move and use your body. They can assess how you are moving and help you find more comfortable ways to move and use your body. They can help you get back to doing things that are important to you like exercise, work, or hobbies. They can work with you 1 to 1 either face to face in the hospital or via telehealth and within group pain management programs and exercise groups.
Our clinical psychologists will explore how you are coping with your pain and its impact on your life (mood, stress, sleep, family, work and leisure activities). They can help you manage unhelpful thoughts that cause distress and lead you away from what you want to be doing. They can help you learn effective strategies for managing pain, such as pacing activities, meditation and flare-up planning.
Hospital pharmacy can tell you about how to take your medicines safely and make sure your pain medicines work with your other medicines.
Our occupational therapist is available to help you to be as independent as you can in your daily functional activities. They may suggest some strategies or aids to help facilitate your independence.
Our social worker is available to help you with practical social and emotional issues that you may experience. They can also provide you with information and education around what other community services are available.
We provide the following services:
Acute pain management
While you are in hospital, our team will help you deal with any pain related to your medical condition, trauma or surgery. Our team visits the wards each day and we are on-call 24 hours a day.
We use a range of medicines to try to relieve pain. Some of them you receive through an infusion. Sometimes you can manage this medicine yourself through a special machine. Other medicines we use include tablets or injections which can help with pain.
Our outpatient clinic for persistent (chronic) pain
Some people experience long term ongoing pain. Our team can work with you to find out what might be causing your pain, how best to minimise it and how you can develop some strategies to cope better with this pain. Treatments include medicines and injections, electrical stimulation devices, exercise therapies, pain education, practicing meditation and relaxation techniques and reviewing your home, leisure and work environments. Some of these are offered to you individually. Others are offered on a group basis. They are generally undertaken in the outpatient setting but some treatments may require a brief stay in hospital.
Pain self-management programs with our Allied Health Team
Persistent pain is best treated by understanding what is happening in your body and nervous system, your psychology (thoughts, beliefs, emotions, habits, ways of coping) and social situation.
We use help you learn strategies such as pacing activity, mindfulness, exercise and healthy living to help treat your pain.
Our process includes:
1. Initial appointment with our doctor, physiotherapist and psychologist to assess your needs. Perhaps further medical treatment and follow-up with the pain doctors.
2. Information session with our physiotherapist, psychologist and pain nurse to help you:
- Make sense of your pain by learning the science of pain.
- Learn about medicines and other options to make good health decisions.
- Understand why your nervous system and natural reactions to pain might be preventing your recovery.
- Learn how active strategies like mindfulness and pacing activity can change the way your nervous system processes information to produce pain. This will allow you to do more with less pain.
- Respond to your pain in helpful ways rather than react in unhelpful ways.
3. Self-directed learning: books, apps, or referral by us to an online course.
4. Mini group workshops with our physiotherapist and psychologist to:
- Build your understanding of pain science.
- Set goals and increase your motivation to improve your mood and quality of life.
- Guide exercise to increase your flexibility, strength and fitness and your ability to move more easily despite pain.
- Pace and simplify activities to improve your day-to-day function without increasing pain.
- Practise mindfulness and desensitisation for managing your pain sensations, unhelpful thoughts and distressing emotions.
5. Further small group workshops - over 8 sessions of 3 hours with our physiotherapist, psychologist and pain nurse. Includes a program of activities between sessions.
- Establish a suitable exercise routine.
- Manage unhelpful thoughts, emotions and behaviours that may be maintaining your pain problem.
- Improve stress and sleep to have more energy and be more able to cope with pain.
- Develop assertive communication skills to get what you need while improving relationships.
- Learn a wide range of pain coping strategies including mindful meditation, desensitisation to manage setbacks and flare-ups so that you are not overwhelmed by pain
6. Individual sessions with a physiotherapist or psychologist if needed to consolidate your use of active self-management strategies. Not for massage or manual treatment. Not for treatment of anxiety, depression, PTSD or other mental illness.
7. Exercise Group – a low intensity group program for people who have completed one of our pain management programs. The number of sessions will be prescribed by our team. This is a stepping stone towards a community exercise program.
Cancer Pain Management
Our team will work with our hospital’s cancer and palliative care teams to help manage your pain from cancer. This may include medication review or adjustments, interventional pain procedures as well as exploring ways of improving pain coping strategies using psychological and exercise approaches.
Complex pain services
Our department is also a referral centre for patients requiring more complex pain assessment and management.
We provide advice and care for people living in regional and remote areas through our telehealth clinic. This means that we communicate with you through a video link on your computer screen. Once we have your referral, we will contact you and discuss how this works.
You will need a referral letter from your local general practitioner (GP) or specialty doctor to use this service. Your doctor will need to submit this referral electronically via Healthlink. Your referral will include your medical history, relevant test results, X-ray results and what medicines you are currently taking.
Once we receive this referral and accept it, we will send you a letter with your appointment details. We will also send this to your doctor. If we cannot make an appointment for you, we will send you a letter confirming that you are on the waiting list for the next available appointment. If you change your address and/or phone number, please call 02 9382 2863.
If you need to change or cancel your appointment or no longer require an appointment, please call 02 9382 2863.
We have many requests for letters to support National Disability Scheme (NDIS) or Disability Support Pension (DSP) applications.
We will write comprehensive letters to your referring doctor. These letters can be used for your NDIS or DSP applications.
We will not write letters to NDIS or Centrelink
Please bring:
- Your Medicare card or Veteran Affairs card
- A list of your medicines including any herbal or over the counter medicines
- Any recent x rays or medical images and their reports
- Insurer details if you are claiming workers compensation, public liability or third party insurance.
When you come to our hospital for your appointment, you can check-in using our electronic check-in kiosks. These are located in our Adult Outpatient Department, Acute Services Building (Botany Street), High Street and Barker Street entrances.

In your first appointment, you may see either a pain specialist alone or a team of specialists including the doctor, clinical psychologist and physiotherapist. If we need to do further assessments, we will arrange another time to do this. We will work with you to develop a pain management plan.
Make an appointment with your local family doctor to talk to them first. If your local doctor needs some advice they can contact us.
Websites on chronic pain
- Chronic Pain Australia www.chronicpainaustralia.org.au
- Pain Australia www.painaustralia.org.au
- Mind Spot www.mindspot.org.au
- This way up Online Treatment Program for Chronic Pain | THIS WAY UP
Brainman brief educational videos:
- Understanding pain in less than 5 minutes, and what to do about it!
- Understanding Pain: Brainman stops his opioids
- Understanding Pain: Brainman chooses
Books on pain
Rewire your pain: an evidence based approach to reduce chronic pain. Davies S, Cooke N, Sutton J.
Explain Pain. Butler, D. S., & Moseley, G. L.
Manage your pain: practical and positive ways of adapting to chronic pain. Nicholas M, Molloy A, Tonkin L, Beeston L.
The Pain Book, finding hope when it hurts. Siddall P, McCabe C, Murray R.
Research
We are dedicated to learning more about what causes pain and more effective ways people can deal with pain. We are also interested in monitoring some of the medicines people use for their pain. We do this in partnership with other research teams and health services.
We may ask you if you would like to be part of our research. You have the right to say no. If you do so, this will not impact on the services we provide to you.
Training and Education
Prince of Wales Hospital is a public teaching hospital. Our department is actively involved in teaching medical students, doctors, nursing and other health care staff about how to best manage pain. We are also accredited with the Faculty of Pain Medicine of the Australian and New Zealand College of Anaesthetists to provide specialist training for doctors to specialise in pain medicine. You may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
Please let us know if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and call us on 02 9382 2963.
Pain Management Department
How we can help you
We help you manage your pain and its impact on your life. We focus on the medical, physical, social, psychological and environmental factors associated with pain.
We can help you develop a plan to:
- reduce how much pain you are feeling
- increase what you can do
- regain control of your life, and
- improve the quality of your life.
Managers
Director A/Prof K E Khor
Nurse Manager David Begley
Opening hours
Pain Clinic days are Monday, Tuesday, Wednesday & Friday.
Learn about our electronic referral system
How to find us
The Prince of Wales Hospital Pain Management Services (and Pain Clinic) are located at: Outpatients Department, Level 2, Campus Centre, Prince of Wales Hospital (Building 16 on our campus map)
Information about how to get to our Randwick campus
We are a team of health professionals, based in the hospital, who will work with you to help you manage your pain.
Our doctors specialise in pain medicine, anaesthesia, geriatric medicine, addiction medicine, psychiatry and rehabilitation medicine. They will help you:
- Understand your pain and what may be causing it
- Reduce your pain using medicines and other treatments
- Maximise what you are able to do when you have pain
- Understand how your pain is affecting your physical and emotional health
- Use prescribed pain medicines safely
- Manage short term experiences of acute pain such as after having surgery.
Our nurses will assess your pain, give you education and pain treatments. Our nurses can help answer questions you have about treatments or medicines. Our nurses also will work with you in our pain programs, focusing on mindfulness and medicines.
Our physiotherapist will have time to explain what is happening when your body is in pain and how that can impact how you move and use your body. They can assess how you are moving and help you find more comfortable ways to move and use your body. They can help you get back to doing things that are important to you like exercise, work, or hobbies. They can work with you 1 to 1 either face to face in the hospital or via telehealth and within group pain management programs and exercise groups.
Our clinical psychologists will explore how you are coping with your pain and its impact on your life (mood, stress, sleep, family, work and leisure activities). They can help you manage unhelpful thoughts that cause distress and lead you away from what you want to be doing. They can help you learn effective strategies for managing pain, such as pacing activities, meditation and flare-up planning.
Hospital pharmacy can tell you about how to take your medicines safely and make sure your pain medicines work with your other medicines.
Our occupational therapist is available to help you to be as independent as you can in your daily functional activities. They may suggest some strategies or aids to help facilitate your independence.
Our social worker is available to help you with practical social and emotional issues that you may experience. They can also provide you with information and education around what other community services are available.
We provide the following services:
Acute pain management
While you are in hospital, our team will help you deal with any pain related to your medical condition, trauma or surgery. Our team visits the wards each day and we are on-call 24 hours a day.
We use a range of medicines to try to relieve pain. Some of them you receive through an infusion. Sometimes you can manage this medicine yourself through a special machine. Other medicines we use include tablets or injections which can help with pain.
Our outpatient clinic for persistent (chronic) pain
Some people experience long term ongoing pain. Our team can work with you to find out what might be causing your pain, how best to minimise it and how you can develop some strategies to cope better with this pain. Treatments include medicines and injections, electrical stimulation devices, exercise therapies, pain education, practicing meditation and relaxation techniques and reviewing your home, leisure and work environments. Some of these are offered to you individually. Others are offered on a group basis. They are generally undertaken in the outpatient setting but some treatments may require a brief stay in hospital.
Pain self-management programs with our Allied Health Team
Persistent pain is best treated by understanding what is happening in your body and nervous system, your psychology (thoughts, beliefs, emotions, habits, ways of coping) and social situation.
We use help you learn strategies such as pacing activity, mindfulness, exercise and healthy living to help treat your pain.
Our process includes:
1. Initial appointment with our doctor, physiotherapist and psychologist to assess your needs. Perhaps further medical treatment and follow-up with the pain doctors.
2. Information session with our physiotherapist, psychologist and pain nurse to help you:
- Make sense of your pain by learning the science of pain.
- Learn about medicines and other options to make good health decisions.
- Understand why your nervous system and natural reactions to pain might be preventing your recovery.
- Learn how active strategies like mindfulness and pacing activity can change the way your nervous system processes information to produce pain. This will allow you to do more with less pain.
- Respond to your pain in helpful ways rather than react in unhelpful ways.
3. Self-directed learning: books, apps, or referral by us to an online course.
4. Mini group workshops with our physiotherapist and psychologist to:
- Build your understanding of pain science.
- Set goals and increase your motivation to improve your mood and quality of life.
- Guide exercise to increase your flexibility, strength and fitness and your ability to move more easily despite pain.
- Pace and simplify activities to improve your day-to-day function without increasing pain.
- Practise mindfulness and desensitisation for managing your pain sensations, unhelpful thoughts and distressing emotions.
5. Further small group workshops - over 8 sessions of 3 hours with our physiotherapist, psychologist and pain nurse. Includes a program of activities between sessions.
- Establish a suitable exercise routine.
- Manage unhelpful thoughts, emotions and behaviours that may be maintaining your pain problem.
- Improve stress and sleep to have more energy and be more able to cope with pain.
- Develop assertive communication skills to get what you need while improving relationships.
- Learn a wide range of pain coping strategies including mindful meditation, desensitisation to manage setbacks and flare-ups so that you are not overwhelmed by pain
6. Individual sessions with a physiotherapist or psychologist if needed to consolidate your use of active self-management strategies. Not for massage or manual treatment. Not for treatment of anxiety, depression, PTSD or other mental illness.
7. Exercise Group – a low intensity group program for people who have completed one of our pain management programs. The number of sessions will be prescribed by our team. This is a stepping stone towards a community exercise program.
Cancer Pain Management
Our team will work with our hospital’s cancer and palliative care teams to help manage your pain from cancer. This may include medication review or adjustments, interventional pain procedures as well as exploring ways of improving pain coping strategies using psychological and exercise approaches.
Complex pain services
Our department is also a referral centre for patients requiring more complex pain assessment and management.
We provide advice and care for people living in regional and remote areas through our telehealth clinic. This means that we communicate with you through a video link on your computer screen. Once we have your referral, we will contact you and discuss how this works.
You will need a referral letter from your local general practitioner (GP) or specialty doctor to use this service. Your doctor will need to submit this referral electronically via Healthlink. Your referral will include your medical history, relevant test results, X-ray results and what medicines you are currently taking.
Once we receive this referral and accept it, we will send you a letter with your appointment details. We will also send this to your doctor. If we cannot make an appointment for you, we will send you a letter confirming that you are on the waiting list for the next available appointment. If you change your address and/or phone number, please call 02 9382 2863.
If you need to change or cancel your appointment or no longer require an appointment, please call 02 9382 2863.
We have many requests for letters to support National Disability Scheme (NDIS) or Disability Support Pension (DSP) applications.
We will write comprehensive letters to your referring doctor. These letters can be used for your NDIS or DSP applications.
We will not write letters to NDIS or Centrelink
Please bring:
- Your Medicare card or Veteran Affairs card
- A list of your medicines including any herbal or over the counter medicines
- Any recent x rays or medical images and their reports
- Insurer details if you are claiming workers compensation, public liability or third party insurance.
When you come to our hospital for your appointment, you can check-in using our electronic check-in kiosks. These are located in our Adult Outpatient Department, Acute Services Building (Botany Street), High Street and Barker Street entrances.

In your first appointment, you may see either a pain specialist alone or a team of specialists including the doctor, clinical psychologist and physiotherapist. If we need to do further assessments, we will arrange another time to do this. We will work with you to develop a pain management plan.
Make an appointment with your local family doctor to talk to them first. If your local doctor needs some advice they can contact us.
Websites on chronic pain
- Chronic Pain Australia www.chronicpainaustralia.org.au
- Pain Australia www.painaustralia.org.au
- Mind Spot www.mindspot.org.au
- This way up Online Treatment Program for Chronic Pain | THIS WAY UP
Brainman brief educational videos:
- Understanding pain in less than 5 minutes, and what to do about it!
- Understanding Pain: Brainman stops his opioids
- Understanding Pain: Brainman chooses
Books on pain
Rewire your pain: an evidence based approach to reduce chronic pain. Davies S, Cooke N, Sutton J.
Explain Pain. Butler, D. S., & Moseley, G. L.
Manage your pain: practical and positive ways of adapting to chronic pain. Nicholas M, Molloy A, Tonkin L, Beeston L.
The Pain Book, finding hope when it hurts. Siddall P, McCabe C, Murray R.
Research
We are dedicated to learning more about what causes pain and more effective ways people can deal with pain. We are also interested in monitoring some of the medicines people use for their pain. We do this in partnership with other research teams and health services.
We may ask you if you would like to be part of our research. You have the right to say no. If you do so, this will not impact on the services we provide to you.
Training and Education
Prince of Wales Hospital is a public teaching hospital. Our department is actively involved in teaching medical students, doctors, nursing and other health care staff about how to best manage pain. We are also accredited with the Faculty of Pain Medicine of the Australian and New Zealand College of Anaesthetists to provide specialist training for doctors to specialise in pain medicine. You may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
Please let us know if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and call us on 02 9382 2963.
Eye Clinic for Prince of Wales Hospital
How we can help you
The Prince of Wales Hospital Eye Clinic is an outpatient clinic which provides comprehensive medical and surgical ophthalmic and orthoptic care to adults with eye related problems.
The Eye Clinic is located on Level 4, High Street Building, Prince of Wales Hospital.
|
Ophthalmic care is given by our ophthalmologists, specialist doctors who can provide diagnosis, medical treatment and complex microsurgery. Orthoptic care is given by our orthopists, eye health professionals who are trained in assessment, diagnosis and non-surgical treatment of problems with eye movement, squint, double vision and lazy eye. |
The Prince of Wales Eye Clinic provide services for adults with the following eye problems:
- Cataracts
- Diabetic eye disorders
- Glaucoma
- Macular degeneration
- Retinal and vitreous disorders and conditions
- Eye emergency and eye trauma treatment
- Cornea
- Cancer of the eye
- Immunology and inflammation of the middle eye (uveitis)
- Neuro-ophthalmology
- Ophthalmic plastic and orbit surgery
We also provide 24 hours a day, 7 days a week emergency care to the Emergency Department of The Prince of Wales Hospital.
Our Outback Eye Service is based in the Department of Ophthalmology at The Prince of Wales Hospital.
The Sydney Children's Hospital Lion’s Eye Clinic is located in the Sydney Children's Hospital main building on Level 0. It provides assessment and treatment for all aspects of paediatric (ie. children aged 16 years and younger) ophthalmology.
Manager
Nursing Manager Michael Cowan
Opening times
8.00am to 4.30pm Monday to Friday
We are closed on weekends and public holidays.
How to find us
Level 4, High St Building, Prince of Wales Hospital (Building 2 on our campus map)
Information about how to get to our Randwick campus
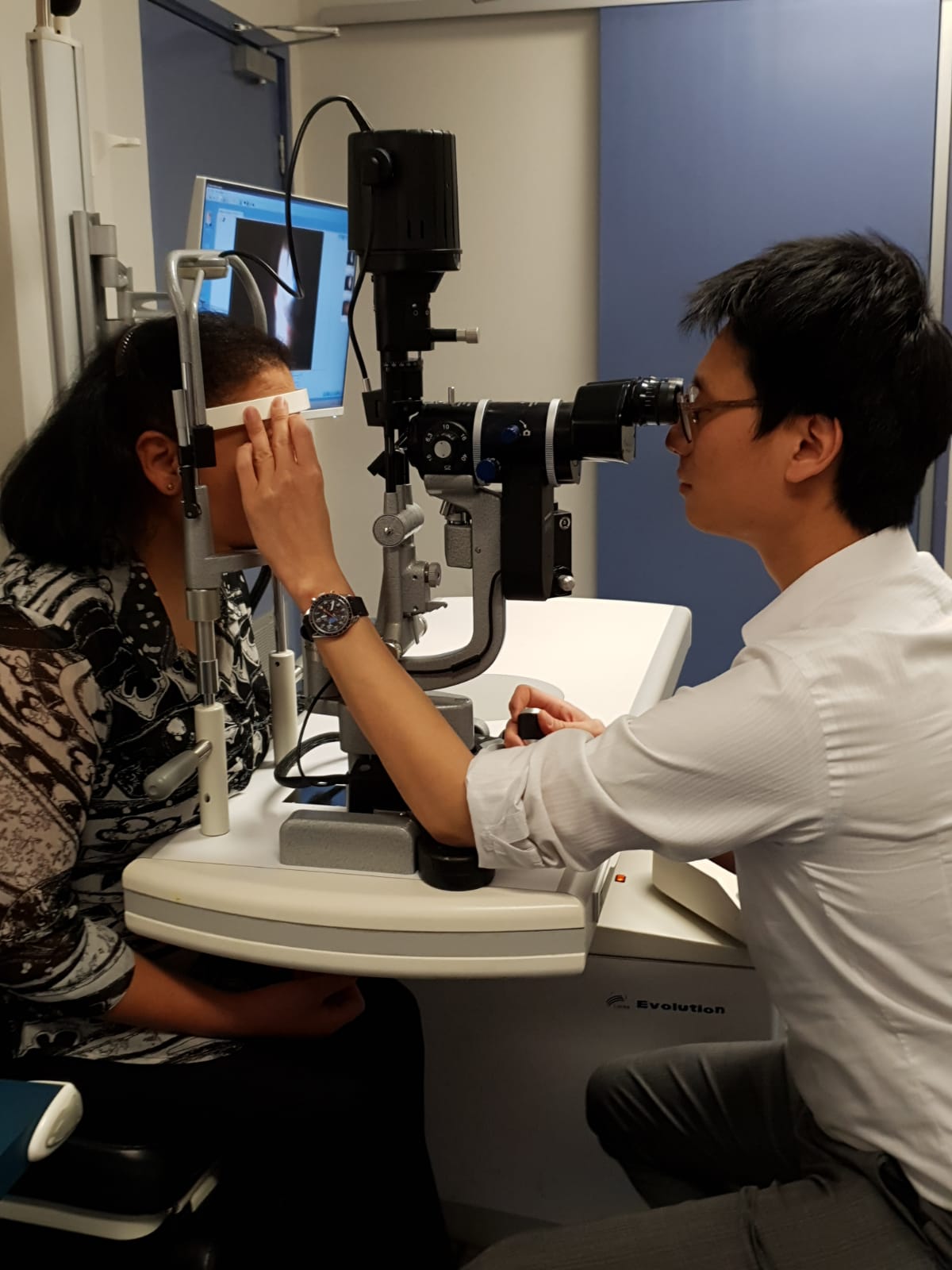
The eye clinic is staffed by:
- Doctors - Specialist Ophthalmologists, Ophthalmology Registrars and Hospital Resident Medical Officer;
- Ophthalmic Nurses
- Orthoptists
- Technical Officers; and
- Clerical and administrative staff.
We work in partnership with your local general practitioner (GP) and both hospital.
If you are new to the eye clinic and have not previously requested an appointment you must have a referral from your local general practitioner (GP) or Optometrist to use our service. They will prepare a written referral for you, which includes a description of the clinical problem.
Please fax, post in the mail or bring the referral letter to our Eye Clinic.
Once we have received your completed referral you will be placed in a wait-list for the next available appointment. When your appointment has been confirmed, we will send you a letter to your home address confirming the date, time and location of your appointment.
Please make sure your referring GP or Optometrist has your current contact details (particularly your address), otherwise we may not be able to contact you with your appointment.
If you are a current patient, please book a follow up appointment at the Eye Clinic reception after your consultation with our Doctor, prior to leaving.
If we have long waiting times for non-urgent conditions and your need is not urgent (e.g. eye check up for prescription glasses) we may make arrangements for you to visit a different service.
To change or cancel your appointment
If you need to change or cancel your appointment, please contact us as soon as possible on 9382 2261, Monday to Friday 8.00am – 4.30pm.
Changing your appointment may mean we need to place you back on the wait-list. You may need to wait to 8-12 months for your next appointment.
To help us with your request please provide the following information when making your change or cancellation request:
- Your full name
- Your Medicare number
- Date of birth
- Telephone number
- The date and time of your original appointment.
If you cannot attend and do not notify us in advance, you will not be automatically given another appointment at the Eye Clinic. You will need to return to your GP or Optometrist to arrange a new referral and new appointment with us.
If any of your contact details change please let us know by phone on 9382 2261 or in person at the Eye Clinic reception.
Please remember to bring to your appointment:
- A list of your current medicines to your appointment
- Details of any previous reactions to eye drops
- Details of your past medical history
- Current glasses
- Eye related problems and treatments.
You will be unable to drive home if you are having dilating eye drops during your appointment. If this is the case please arrange alternative transport home after your appointment.
Your visit to the Eye Clinic may involve these steps:
1. Check-in
Please go to the Eye Clinic reception to check-in. Our administration staff will confirm that your contact details (in particular your address) are up to date on our records. Please do not arrive earlier than 15 minutes prior to your appointment time.
2. Initial eye assessment
After checking-in, you will be asked to wait in the waiting room for your initial eye assessment.
Your eye assessment may involve various staff (eg. Orthoptists and Ophthalmic nurses), who each have differing roles to play in relation to your eye testing. The relevant staff members will introduce themselves to you by name, and describe their role in your eye assessment.
Each time you meet a new staff member we will ask you about any previous adverse reactions you have had to eye drops (if you needed them). Our staff will also ask you to describe your symptoms and your past medical history and also any eye problems and treatments you have had.
Eye assessments often involve the use of eye drops to determine your eye pressure, or to dilate your pupils so that the internal structure of your eyes can be examined. This can take up to 20 minutes to take effect.
You may need a number of tests and need to wait on the availability of the specialised equipment that we use and the availability of staff to perform these tests for you.
3. Eye consultation
After the eye assessment has been performed, you will be seen by the Ophthalmology Consultant or Registrar doctor to discuss your symptoms and treatment.
4. Booking follow-up appointment (if required)
After meeting with the Ophthalmology Consultant or Registrar doctor you may need to go to the Eye Clinic Reception desk to book a follow-up appointment before leaving the clinic.
5. Going home
We recommend you organise someone else to drive you home. If you are given dilating drops your eyesight can be blurred and you will be more sensitive to light for a few hours.
A visit to our eye clinic can often take several hours. Please do not check-in earlier than 15 minutes prior to your appointment time.
Our services are shared between eye clinic outpatients, hospital inpatients, emergencies in our Emergency Department, operating theatres and other services. We always treat patients on the basis of clinical urgency and at times our medical staff may be called away to attend urgent cases. If there is a delay we will let you know when you check-in. Occasionally, we may need to reschedule your appointment.
We appreciate your patience in circumstances where wait-times are longer than expected.
If you are told you will need to continue to use eye drops after leaving our clinic you will be given an initial supply plus a prescription to get more from your pharmacy. If you need further prescriptions, you will need to organise this with your local GP. We suggest you take an eye drop bottle with you to show them.
Sometimes it can take several weeks before your GP and/or Optometrist (who referred you to the Eye Clinic) receives the letter explaining your visit to our clinic. explaining your diagnosis, treatment plan and follow up arrangements. It is important for you to understand your eye condition, the treatment required, and follow up arrangements prior to leaving our clinic.
If you experience an unexpected or urgent eye problem between appointments, please contact:
- The Eye Clinic on 9382 2261 (Press option 2, then 4), during our opening hours, or
- Your General Practitioner or Optometrist, or
- The nearest Hospital Emergency Department (if an emergency).
Please let us know at least 30 days before your appointment if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and the healthcare professional you want to speak with.
We are teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
We appreciate your feedback. If you would like to give us feedback on our services please complete a feedback form when you come to an appointment.
Eye Clinic for Prince of Wales Hospital
How we can help you
The Prince of Wales Hospital Eye Clinic is an outpatient clinic which provides comprehensive medical and surgical ophthalmic and orthoptic care to adults with eye related problems.
The Eye Clinic is located on Level 4, High Street Building, Prince of Wales Hospital.
|
Ophthalmic care is given by our ophthalmologists, specialist doctors who can provide diagnosis, medical treatment and complex microsurgery. Orthoptic care is given by our orthopists, eye health professionals who are trained in assessment, diagnosis and non-surgical treatment of problems with eye movement, squint, double vision and lazy eye. |
The Prince of Wales Eye Clinic provide services for adults with the following eye problems:
- Cataracts
- Diabetic eye disorders
- Glaucoma
- Macular degeneration
- Retinal and vitreous disorders and conditions
- Eye emergency and eye trauma treatment
- Cornea
- Cancer of the eye
- Immunology and inflammation of the middle eye (uveitis)
- Neuro-ophthalmology
- Ophthalmic plastic and orbit surgery
We also provide 24 hours a day, 7 days a week emergency care to the Emergency Department of The Prince of Wales Hospital.
Our Outback Eye Service is based in the Department of Ophthalmology at The Prince of Wales Hospital.
The Sydney Children's Hospital Lion’s Eye Clinic is located in the Sydney Children's Hospital main building on Level 0. It provides assessment and treatment for all aspects of paediatric (ie. children aged 16 years and younger) ophthalmology.
Manager
Nursing Manager Michael Cowan
Opening times
8.00am to 4.30pm Monday to Friday
We are closed on weekends and public holidays.
How to find us
Level 4, High St Building, Prince of Wales Hospital (Building 2 on our campus map)
Information about how to get to our Randwick campus
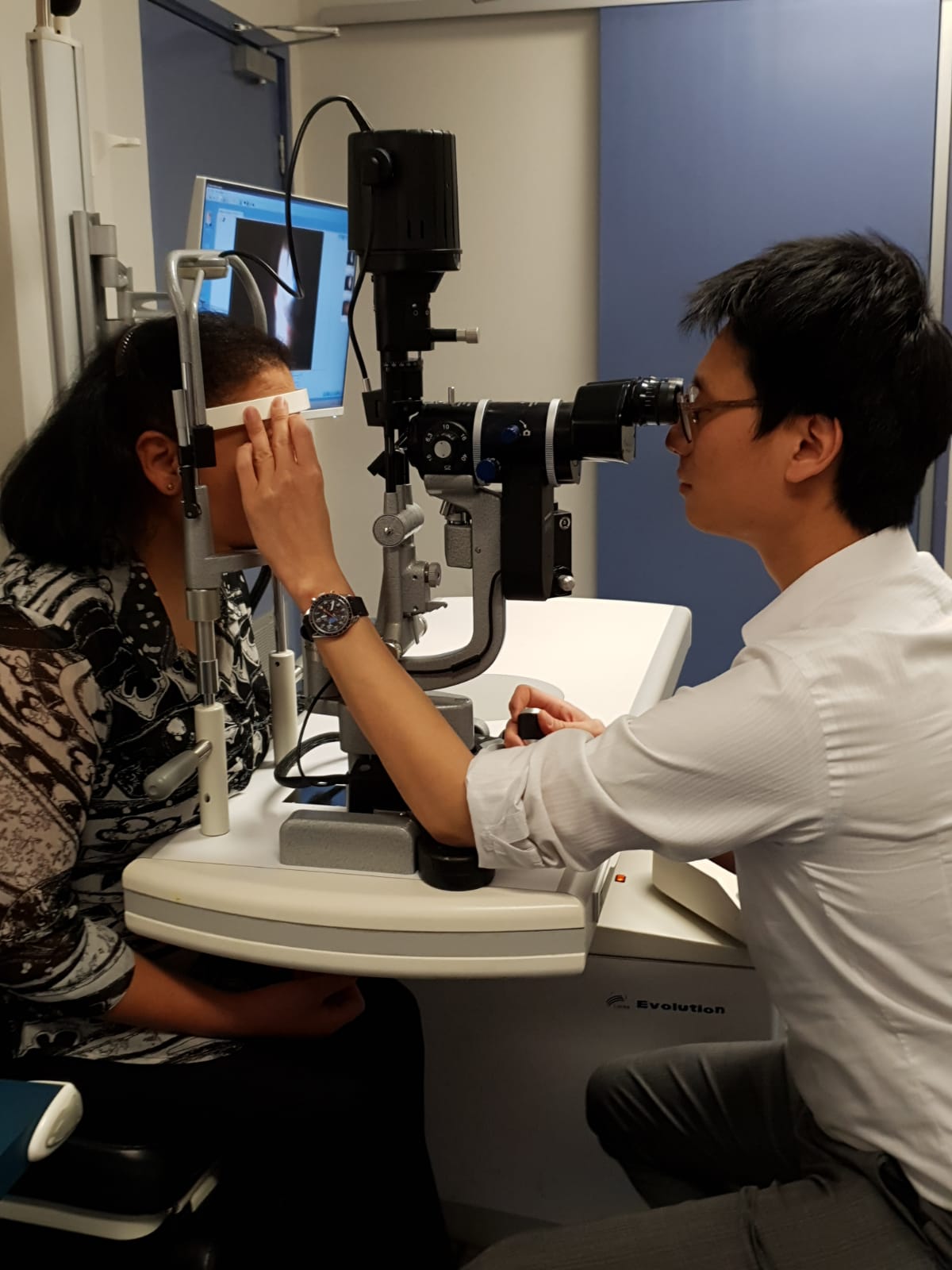
The eye clinic is staffed by:
- Doctors - Specialist Ophthalmologists, Ophthalmology Registrars and Hospital Resident Medical Officer;
- Ophthalmic Nurses
- Orthoptists
- Technical Officers; and
- Clerical and administrative staff.
We work in partnership with your local general practitioner (GP) and both hospital.
If you are new to the eye clinic and have not previously requested an appointment you must have a referral from your local general practitioner (GP) or Optometrist to use our service. They will prepare a written referral for you, which includes a description of the clinical problem.
Please fax, post in the mail or bring the referral letter to our Eye Clinic.
Once we have received your completed referral you will be placed in a wait-list for the next available appointment. When your appointment has been confirmed, we will send you a letter to your home address confirming the date, time and location of your appointment.
Please make sure your referring GP or Optometrist has your current contact details (particularly your address), otherwise we may not be able to contact you with your appointment.
If you are a current patient, please book a follow up appointment at the Eye Clinic reception after your consultation with our Doctor, prior to leaving.
If we have long waiting times for non-urgent conditions and your need is not urgent (e.g. eye check up for prescription glasses) we may make arrangements for you to visit a different service.
To change or cancel your appointment
If you need to change or cancel your appointment, please contact us as soon as possible on 9382 2261, Monday to Friday 8.00am – 4.30pm.
Changing your appointment may mean we need to place you back on the wait-list. You may need to wait to 8-12 months for your next appointment.
To help us with your request please provide the following information when making your change or cancellation request:
- Your full name
- Your Medicare number
- Date of birth
- Telephone number
- The date and time of your original appointment.
If you cannot attend and do not notify us in advance, you will not be automatically given another appointment at the Eye Clinic. You will need to return to your GP or Optometrist to arrange a new referral and new appointment with us.
If any of your contact details change please let us know by phone on 9382 2261 or in person at the Eye Clinic reception.
Please remember to bring to your appointment:
- A list of your current medicines to your appointment
- Details of any previous reactions to eye drops
- Details of your past medical history
- Current glasses
- Eye related problems and treatments.
You will be unable to drive home if you are having dilating eye drops during your appointment. If this is the case please arrange alternative transport home after your appointment.
Your visit to the Eye Clinic may involve these steps:
1. Check-in
Please go to the Eye Clinic reception to check-in. Our administration staff will confirm that your contact details (in particular your address) are up to date on our records. Please do not arrive earlier than 15 minutes prior to your appointment time.
2. Initial eye assessment
After checking-in, you will be asked to wait in the waiting room for your initial eye assessment.
Your eye assessment may involve various staff (eg. Orthoptists and Ophthalmic nurses), who each have differing roles to play in relation to your eye testing. The relevant staff members will introduce themselves to you by name, and describe their role in your eye assessment.
Each time you meet a new staff member we will ask you about any previous adverse reactions you have had to eye drops (if you needed them). Our staff will also ask you to describe your symptoms and your past medical history and also any eye problems and treatments you have had.
Eye assessments often involve the use of eye drops to determine your eye pressure, or to dilate your pupils so that the internal structure of your eyes can be examined. This can take up to 20 minutes to take effect.
You may need a number of tests and need to wait on the availability of the specialised equipment that we use and the availability of staff to perform these tests for you.
3. Eye consultation
After the eye assessment has been performed, you will be seen by the Ophthalmology Consultant or Registrar doctor to discuss your symptoms and treatment.
4. Booking follow-up appointment (if required)
After meeting with the Ophthalmology Consultant or Registrar doctor you may need to go to the Eye Clinic Reception desk to book a follow-up appointment before leaving the clinic.
5. Going home
We recommend you organise someone else to drive you home. If you are given dilating drops your eyesight can be blurred and you will be more sensitive to light for a few hours.
A visit to our eye clinic can often take several hours. Please do not check-in earlier than 15 minutes prior to your appointment time.
Our services are shared between eye clinic outpatients, hospital inpatients, emergencies in our Emergency Department, operating theatres and other services. We always treat patients on the basis of clinical urgency and at times our medical staff may be called away to attend urgent cases. If there is a delay we will let you know when you check-in. Occasionally, we may need to reschedule your appointment.
We appreciate your patience in circumstances where wait-times are longer than expected.
If you are told you will need to continue to use eye drops after leaving our clinic you will be given an initial supply plus a prescription to get more from your pharmacy. If you need further prescriptions, you will need to organise this with your local GP. We suggest you take an eye drop bottle with you to show them.
Sometimes it can take several weeks before your GP and/or Optometrist (who referred you to the Eye Clinic) receives the letter explaining your visit to our clinic. explaining your diagnosis, treatment plan and follow up arrangements. It is important for you to understand your eye condition, the treatment required, and follow up arrangements prior to leaving our clinic.
If you experience an unexpected or urgent eye problem between appointments, please contact:
- The Eye Clinic on 9382 2261 (Press option 2, then 4), during our opening hours, or
- Your General Practitioner or Optometrist, or
- The nearest Hospital Emergency Department (if an emergency).
Please let us know at least 30 days before your appointment if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and the healthcare professional you want to speak with.
We are teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
We appreciate your feedback. If you would like to give us feedback on our services please complete a feedback form when you come to an appointment.
Eye Clinic for Prince of Wales Hospital
How we can help you
The Prince of Wales Hospital Eye Clinic is an outpatient clinic which provides comprehensive medical and surgical ophthalmic and orthoptic care to adults with eye related problems.
The Eye Clinic is located on Level 4, High Street Building, Prince of Wales Hospital.
|
Ophthalmic care is given by our ophthalmologists, specialist doctors who can provide diagnosis, medical treatment and complex microsurgery. Orthoptic care is given by our orthopists, eye health professionals who are trained in assessment, diagnosis and non-surgical treatment of problems with eye movement, squint, double vision and lazy eye. |
The Prince of Wales Eye Clinic provide services for adults with the following eye problems:
- Cataracts
- Diabetic eye disorders
- Glaucoma
- Macular degeneration
- Retinal and vitreous disorders and conditions
- Eye emergency and eye trauma treatment
- Cornea
- Cancer of the eye
- Immunology and inflammation of the middle eye (uveitis)
- Neuro-ophthalmology
- Ophthalmic plastic and orbit surgery
We also provide 24 hours a day, 7 days a week emergency care to the Emergency Department of The Prince of Wales Hospital.
Our Outback Eye Service is based in the Department of Ophthalmology at The Prince of Wales Hospital.
The Sydney Children's Hospital Lion’s Eye Clinic is located in the Sydney Children's Hospital main building on Level 0. It provides assessment and treatment for all aspects of paediatric (ie. children aged 16 years and younger) ophthalmology.
Manager
Nursing Manager Michael Cowan
Opening times
8.00am to 4.30pm Monday to Friday
We are closed on weekends and public holidays.
How to find us
Level 4, High St Building, Prince of Wales Hospital (Building 2 on our campus map)
Information about how to get to our Randwick campus
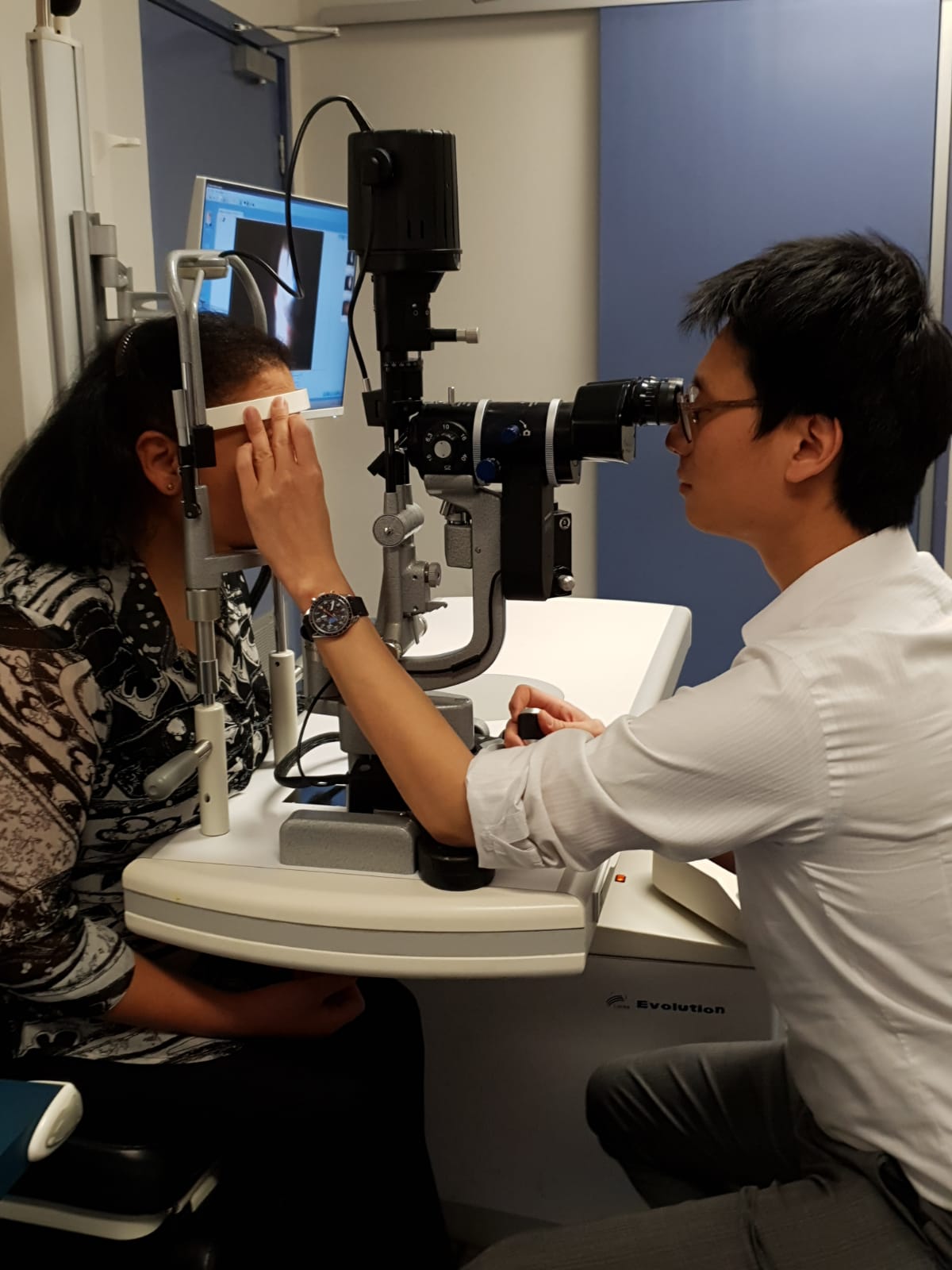
The eye clinic is staffed by:
- Doctors - Specialist Ophthalmologists, Ophthalmology Registrars and Hospital Resident Medical Officer;
- Ophthalmic Nurses
- Orthoptists
- Technical Officers; and
- Clerical and administrative staff.
We work in partnership with your local general practitioner (GP) and both hospital.
If you are new to the eye clinic and have not previously requested an appointment you must have a referral from your local general practitioner (GP) or Optometrist to use our service. They will prepare a written referral for you, which includes a description of the clinical problem.
Please fax, post in the mail or bring the referral letter to our Eye Clinic.
Once we have received your completed referral you will be placed in a wait-list for the next available appointment. When your appointment has been confirmed, we will send you a letter to your home address confirming the date, time and location of your appointment.
Please make sure your referring GP or Optometrist has your current contact details (particularly your address), otherwise we may not be able to contact you with your appointment.
If you are a current patient, please book a follow up appointment at the Eye Clinic reception after your consultation with our Doctor, prior to leaving.
If we have long waiting times for non-urgent conditions and your need is not urgent (e.g. eye check up for prescription glasses) we may make arrangements for you to visit a different service.
To change or cancel your appointment
If you need to change or cancel your appointment, please contact us as soon as possible on 9382 2261, Monday to Friday 8.00am – 4.30pm.
Changing your appointment may mean we need to place you back on the wait-list. You may need to wait to 8-12 months for your next appointment.
To help us with your request please provide the following information when making your change or cancellation request:
- Your full name
- Your Medicare number
- Date of birth
- Telephone number
- The date and time of your original appointment.
If you cannot attend and do not notify us in advance, you will not be automatically given another appointment at the Eye Clinic. You will need to return to your GP or Optometrist to arrange a new referral and new appointment with us.
If any of your contact details change please let us know by phone on 9382 2261 or in person at the Eye Clinic reception.
Please remember to bring to your appointment:
- A list of your current medicines to your appointment
- Details of any previous reactions to eye drops
- Details of your past medical history
- Current glasses
- Eye related problems and treatments.
You will be unable to drive home if you are having dilating eye drops during your appointment. If this is the case please arrange alternative transport home after your appointment.
Your visit to the Eye Clinic may involve these steps:
1. Check-in
Please go to the Eye Clinic reception to check-in. Our administration staff will confirm that your contact details (in particular your address) are up to date on our records. Please do not arrive earlier than 15 minutes prior to your appointment time.
2. Initial eye assessment
After checking-in, you will be asked to wait in the waiting room for your initial eye assessment.
Your eye assessment may involve various staff (eg. Orthoptists and Ophthalmic nurses), who each have differing roles to play in relation to your eye testing. The relevant staff members will introduce themselves to you by name, and describe their role in your eye assessment.
Each time you meet a new staff member we will ask you about any previous adverse reactions you have had to eye drops (if you needed them). Our staff will also ask you to describe your symptoms and your past medical history and also any eye problems and treatments you have had.
Eye assessments often involve the use of eye drops to determine your eye pressure, or to dilate your pupils so that the internal structure of your eyes can be examined. This can take up to 20 minutes to take effect.
You may need a number of tests and need to wait on the availability of the specialised equipment that we use and the availability of staff to perform these tests for you.
3. Eye consultation
After the eye assessment has been performed, you will be seen by the Ophthalmology Consultant or Registrar doctor to discuss your symptoms and treatment.
4. Booking follow-up appointment (if required)
After meeting with the Ophthalmology Consultant or Registrar doctor you may need to go to the Eye Clinic Reception desk to book a follow-up appointment before leaving the clinic.
5. Going home
We recommend you organise someone else to drive you home. If you are given dilating drops your eyesight can be blurred and you will be more sensitive to light for a few hours.
A visit to our eye clinic can often take several hours. Please do not check-in earlier than 15 minutes prior to your appointment time.
Our services are shared between eye clinic outpatients, hospital inpatients, emergencies in our Emergency Department, operating theatres and other services. We always treat patients on the basis of clinical urgency and at times our medical staff may be called away to attend urgent cases. If there is a delay we will let you know when you check-in. Occasionally, we may need to reschedule your appointment.
We appreciate your patience in circumstances where wait-times are longer than expected.
If you are told you will need to continue to use eye drops after leaving our clinic you will be given an initial supply plus a prescription to get more from your pharmacy. If you need further prescriptions, you will need to organise this with your local GP. We suggest you take an eye drop bottle with you to show them.
Sometimes it can take several weeks before your GP and/or Optometrist (who referred you to the Eye Clinic) receives the letter explaining your visit to our clinic. explaining your diagnosis, treatment plan and follow up arrangements. It is important for you to understand your eye condition, the treatment required, and follow up arrangements prior to leaving our clinic.
If you experience an unexpected or urgent eye problem between appointments, please contact:
- The Eye Clinic on 9382 2261 (Press option 2, then 4), during our opening hours, or
- Your General Practitioner or Optometrist, or
- The nearest Hospital Emergency Department (if an emergency).
Please let us know at least 30 days before your appointment if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and the healthcare professional you want to speak with.
We are teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
We appreciate your feedback. If you would like to give us feedback on our services please complete a feedback form when you come to an appointment.
Infectious Diseases Department
How we can help you
We provide specialist care for patients with infectious disease who are in hospital or who come to our clinics from the community. Our patients have a broad range of infections, they might have a skin, urine or chest infection, a long term virus or an infection after their surgery.
Our services include:
- care for patients at Prince of Wales Hospital, Royal Hospital for Women and Sydney, Sydney Eye Hospital
- outpatient clinics for patient in the community to visit us
- HIV and hepatitis clinics
- Hepatitis and infectious diseases services at Long Bay Prison.
Learn more about our Respiratory and Infectious Diseases Ward.
Opening hours
8.30 am - 4.00 pm
Learn about our electronic referral system
How to find us
Level 4, Dickinson Building, Prince of Wales Hospital (Building 15 on our campus map)
Information about how to get to our Randwick campus

Our team includes doctors who are specialists in infectious diseases, as well as doctors in training who can assess, diagnose and treat your infection. Our doctors work closely with specialist nurses and allied health staff to provide a high level of care, education and support for our patients.
We have specialist infectious diseases clinics for those living in the community. Our clinics are available four afternoons per week by the following specialists:
| Day | Doctor/Clinic | Location | Phone | Fax |
| Monday |
Dr Mrudhula Asoga |
Adult Outpatient Department | 9382 0400 | 9382 0422 |
| Tuesday |
Dr Trine Gulholm Dr Marianne Martinello |
Level 4, Dickinson Building | 9382 3405 | 9382 3403 |
| Wednesday |
Dr Josh Kim Dr Parth Solanki |
Level 4, Dickinson Building | 9382 3405 | 9382 3403 |
| Thursday | Hospital in the home patients | Level 4, Dickinson Building | 9382 3405 | |
| Friday | Dr Kristen Overton | Level 4, Dickinson Building | 9382 3405 | 9382 3403 |
Patients who are seeking care for viruses in their blood (HIV or Hepatitis) are seen in Tuesday and Friday clinics.
You will need a referral letter from your local general practitioner (GP) or specialty doctor to use this service. Your doctor will need to submit this referral electronically via Healthlink. Your referral will include your medical history, relevant test results, X-ray results and what medicines you are currently taking.
Once we receive this referral and accept it we will send you a letter with your appointment details. We will also send this to your doctor. If we cannot make an appointment for you, we will send you a letter confirming that you are on the waiting list for the next available appointment. If you change your address and/or phone number, please call the appropriate number above.
If you need to change or cancel your appointment or no longer require an appointment/be on the waitlist, please call the appropriate number above.
If you provide your mobile phone number you will receive a SMS reminder two days before your appointment.
Please bring:
- Your referral letter from your GP if it hasn’t already been faxed
- Any recent blood test results (if you do not have a copy of your results, please bring the name of the pathology company that performed the test so we can follow up with them)
- Your Medicare card
- A list of your medicines or bring all your medicines in a bag, including any herbal or over the counter
- You are welcome to bring a support person (a relative, friend or carer) with you.
When you come to our hospital for your appointment, you can check-in using our electronic check-in kiosks. These are located in our Adult Outpatient Department, Acute Services Building (Botany Street), High Street and Barker Street entrances.

We are a teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will not impact in any way on the services we will provide.
Please let us know if you need an interpreter before the date of your appointment. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and call the appropriate number above.
Infectious Diseases Department
How we can help you
We provide specialist care for patients with infectious disease who are in hospital or who come to our clinics from the community. Our patients have a broad range of infections, they might have a skin, urine or chest infection, a long term virus or an infection after their surgery.
Our services include:
- care for patients at Prince of Wales Hospital, Royal Hospital for Women and Sydney, Sydney Eye Hospital
- outpatient clinics for patient in the community to visit us
- HIV and hepatitis clinics
- Hepatitis and infectious diseases services at Long Bay Prison.
Learn more about our Respiratory and Infectious Diseases Ward.
Opening hours
8.30 am - 4.00 pm
Learn about our electronic referral system
How to find us
Level 4, Dickinson Building, Prince of Wales Hospital (Building 15 on our campus map)
Information about how to get to our Randwick campus

Our team includes doctors who are specialists in infectious diseases, as well as doctors in training who can assess, diagnose and treat your infection. Our doctors work closely with specialist nurses and allied health staff to provide a high level of care, education and support for our patients.
We have specialist infectious diseases clinics for those living in the community. Our clinics are available four afternoons per week by the following specialists:
| Day | Doctor/Clinic | Location | Phone | Fax |
| Monday |
Dr Mrudhula Asoga |
Adult Outpatient Department | 9382 0400 | 9382 0422 |
| Tuesday |
Dr Trine Gulholm Dr Marianne Martinello |
Level 4, Dickinson Building | 9382 3405 | 9382 3403 |
| Wednesday |
Dr Josh Kim Dr Parth Solanki |
Level 4, Dickinson Building | 9382 3405 | 9382 3403 |
| Thursday | Hospital in the home patients | Level 4, Dickinson Building | 9382 3405 | |
| Friday | Dr Kristen Overton | Level 4, Dickinson Building | 9382 3405 | 9382 3403 |
Patients who are seeking care for viruses in their blood (HIV or Hepatitis) are seen in Tuesday and Friday clinics.
You will need a referral letter from your local general practitioner (GP) or specialty doctor to use this service. Your doctor will need to submit this referral electronically via Healthlink. Your referral will include your medical history, relevant test results, X-ray results and what medicines you are currently taking.
Once we receive this referral and accept it we will send you a letter with your appointment details. We will also send this to your doctor. If we cannot make an appointment for you, we will send you a letter confirming that you are on the waiting list for the next available appointment. If you change your address and/or phone number, please call the appropriate number above.
If you need to change or cancel your appointment or no longer require an appointment/be on the waitlist, please call the appropriate number above.
If you provide your mobile phone number you will receive a SMS reminder two days before your appointment.
Please bring:
- Your referral letter from your GP if it hasn’t already been faxed
- Any recent blood test results (if you do not have a copy of your results, please bring the name of the pathology company that performed the test so we can follow up with them)
- Your Medicare card
- A list of your medicines or bring all your medicines in a bag, including any herbal or over the counter
- You are welcome to bring a support person (a relative, friend or carer) with you.
When you come to our hospital for your appointment, you can check-in using our electronic check-in kiosks. These are located in our Adult Outpatient Department, Acute Services Building (Botany Street), High Street and Barker Street entrances.

We are a teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will not impact in any way on the services we will provide.
Please let us know if you need an interpreter before the date of your appointment. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and call the appropriate number above.