Endocrine Department
Our Clinics
We provide specialist medical service for people with endocrine problems. These include:
- Osteoporosis and metabolic bone disorders
- Parathyroid & calcium disorders
- Hypertension due to adrenal disorders
- Disorders of the ovary (such as polycystic ovarian syndrome) and some disorders of the testes
- Thyroid disorders (eg goitre, hyperthyroidism, hypothyroidism, thyroiditis, thyroid cancer)
- Pituitary disorders
- Tumours of an endocrine gland.
The endocrine system is made up of glands throughout the body including the hypothalamus, pituitary gland, thyroid, parathyroid, adrenal glands, pancreas, ovaries and testes. Endocrine glands make hormones (chemical messages) allowing communication between various parts of the body. Endocrinology is the study of how these organs work and any resulting problems.
Endocrine problems can occur when there is too much or too little hormone secretion causing an imbalance.
Manager
Director of the Department of Endocrinology, Diabetes and Metabolism, Dr Sue Mei Lau
Learn about our electronic referral system
How to find us
Endocrine Department
Level 2, High Street Building, Prince of Wales Hospital (Building 2B on our campus map)
Endocrine Clinics
Outpatient’s A, Level 2, Campus Centre, Prince of Wales Hospital (Building 16 on our campus map)
Phone: 02 9382 0400
Bone Mineral Density Unit
Located at the Royal Hospital for Women (Building 17 on our campus map). Go to the enquires counter and ask for directions.
Our team includes specialist endocrinologists and doctors in training who assess, treat and help you to manage your endocrine condition.
We work closely with endocrine surgeons, nuclear physicians and pituitary surgeons.
This main role of this service is to measure your bone density to check if you have osteoporosis. We support people who have osteoporosis or are at a risk of developing a bone problem.
There are a number of different ways that osteoporosis is diagnosed. The main method of measuring bone mineral density (the amount of mineral and tissues in a certain volume of bone) is using DEXA analysis, a highly filtered and modified X-ray technique where a small amount of radiation is passed through the body. The amount that is absorbed by the body is proportional to the amount of fat, muscle, soft tissue and bone that is in the path of the two beams (hence the term Dual Energy X-ray Absorptiometry or DEXA). The absorption from fat and other soft tissues is then subtracted to determine the proportion of bone mineral you have.
Other radiological techniques include Quantitative Computerised Axial Tomography (QCT) scanning and vertebral morphometry using a plain lateral spine X-ray of the thoracolumbar region.
For more information on osteoporosis visit www.osteoporosis.org.au
For further information and bookings please call 9382 6617 or fax 9382 6210.
Endocrine dynamic function testing involves collecting two or more blood samples to determine if there are any problems with the function of an endocrine gland. The Endocrine dynamic function team includes an endocrine nurse and endocrine medical registrars.
To make an appointment for your test please telephone the Endocrine Nurse on 938 24680, or Administrative Assistant on 9382 4602. They will give you all the information you need to prepare for your test.
We provide specialised endocrine clinics for the following conditions:
- Thyroid disease including goitre, thyroid nodules, hyperthyroidism, hypothyroidism, thyroid cancer
- Pituitary and hypothalamic disease including pituitary adenomas and cysts, Cushing's disease, acromegaly, prolactinoma, hypopituitarism, hypophysitis.
- Osteoporosis and metabolic disease including hypercalcaemia, hypocalcaemia, Paget's disease, osteomalacia, osteodystrophy.
- Adrenal disease including adrenal related hypertension, congenital adrenal hyperplasia, adrenal adenomas
- Gonadal diseases including Polycystic ovarian syndrome, testosterone deficiency
- Hereditary endocrine cancer syndromes including VHL, MEN I, MEN II
These clinics are held on Mondays and Thursdays in our outpatients department.
We also provide specialised diabetes clinics. For information on these please see our Diabetes Centre page.
You will need a referral letter from your local general practitioner (GP) or specialty doctor to use this service. Your doctor will need to submit this referral electronically via Healthlink. Your referral will include your medical history, relevant test results, X-ray results and what medicines you are currently taking.
Once we receive this referral and accept it we will send you a letter with your appointment details. We will also send this to your doctor. If we cannot make an appointment for you, we will send you a letter confirming that you are on the waiting list for the next available appointment.
If you provide your mobile phone number you will receive a SMS reminder 5 days before your appointment.
If your address or phone number changes or if you need to change or cancel your appointment please telephone the appropriate phone numbers below during business hours:
Specialised endocrine clinics on Tel: 9382 4602
Specialised diabetes clinics on Tel: 9382 4600
Please bring
- Recent blood test results. If you do not have a copy of your results, please bring the name of the pathology company that performed the test so we can follow up with them.
- Any scans and reports related to your hormone condition.
- A list of all the medicines you are currently taking including any herbal or over the counter medicines.
When you come to our hospital for your appointment, you can check-in using our electronic check-in kiosks. These are located in our Adult Outpatient Department, Acute Services Building (Botany Street), High Street and Barker Street entrances.

Please let us know if you need an interpreter before your appointment date. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and call:
Specialised endocrine clinics on Tel: 9382 4602
Specialised diabetes clinics on Tel: 9382 4600
Endocrine Department
Our Clinics
We provide specialist medical service for people with endocrine problems. These include:
- Osteoporosis and metabolic bone disorders
- Parathyroid & calcium disorders
- Hypertension due to adrenal disorders
- Disorders of the ovary (such as polycystic ovarian syndrome) and some disorders of the testes
- Thyroid disorders (eg goitre, hyperthyroidism, hypothyroidism, thyroiditis, thyroid cancer)
- Pituitary disorders
- Tumours of an endocrine gland.
The endocrine system is made up of glands throughout the body including the hypothalamus, pituitary gland, thyroid, parathyroid, adrenal glands, pancreas, ovaries and testes. Endocrine glands make hormones (chemical messages) allowing communication between various parts of the body. Endocrinology is the study of how these organs work and any resulting problems.
Endocrine problems can occur when there is too much or too little hormone secretion causing an imbalance.
Manager
Director of the Department of Endocrinology, Diabetes and Metabolism, Dr Sue Mei Lau
Learn about our electronic referral system
How to find us
Endocrine Department
Level 2, High Street Building, Prince of Wales Hospital (Building 2B on our campus map)
Endocrine Clinics
Outpatient’s A, Level 2, Campus Centre, Prince of Wales Hospital (Building 16 on our campus map)
Phone: 02 9382 0400
Bone Mineral Density Unit
Located at the Royal Hospital for Women (Building 17 on our campus map). Go to the enquires counter and ask for directions.
Our team includes specialist endocrinologists and doctors in training who assess, treat and help you to manage your endocrine condition.
We work closely with endocrine surgeons, nuclear physicians and pituitary surgeons.
This main role of this service is to measure your bone density to check if you have osteoporosis. We support people who have osteoporosis or are at a risk of developing a bone problem.
There are a number of different ways that osteoporosis is diagnosed. The main method of measuring bone mineral density (the amount of mineral and tissues in a certain volume of bone) is using DEXA analysis, a highly filtered and modified X-ray technique where a small amount of radiation is passed through the body. The amount that is absorbed by the body is proportional to the amount of fat, muscle, soft tissue and bone that is in the path of the two beams (hence the term Dual Energy X-ray Absorptiometry or DEXA). The absorption from fat and other soft tissues is then subtracted to determine the proportion of bone mineral you have.
Other radiological techniques include Quantitative Computerised Axial Tomography (QCT) scanning and vertebral morphometry using a plain lateral spine X-ray of the thoracolumbar region.
For more information on osteoporosis visit www.osteoporosis.org.au
For further information and bookings please call 9382 6617 or fax 9382 6210.
Endocrine dynamic function testing involves collecting two or more blood samples to determine if there are any problems with the function of an endocrine gland. The Endocrine dynamic function team includes an endocrine nurse and endocrine medical registrars.
To make an appointment for your test please telephone the Endocrine Nurse on 938 24680, or Administrative Assistant on 9382 4602. They will give you all the information you need to prepare for your test.
We provide specialised endocrine clinics for the following conditions:
- Thyroid disease including goitre, thyroid nodules, hyperthyroidism, hypothyroidism, thyroid cancer
- Pituitary and hypothalamic disease including pituitary adenomas and cysts, Cushing's disease, acromegaly, prolactinoma, hypopituitarism, hypophysitis.
- Osteoporosis and metabolic disease including hypercalcaemia, hypocalcaemia, Paget's disease, osteomalacia, osteodystrophy.
- Adrenal disease including adrenal related hypertension, congenital adrenal hyperplasia, adrenal adenomas
- Gonadal diseases including Polycystic ovarian syndrome, testosterone deficiency
- Hereditary endocrine cancer syndromes including VHL, MEN I, MEN II
These clinics are held on Mondays and Thursdays in our outpatients department.
We also provide specialised diabetes clinics. For information on these please see our Diabetes Centre page.
You will need a referral letter from your local general practitioner (GP) or specialty doctor to use this service. Your doctor will need to submit this referral electronically via Healthlink. Your referral will include your medical history, relevant test results, X-ray results and what medicines you are currently taking.
Once we receive this referral and accept it we will send you a letter with your appointment details. We will also send this to your doctor. If we cannot make an appointment for you, we will send you a letter confirming that you are on the waiting list for the next available appointment.
If you provide your mobile phone number you will receive a SMS reminder 5 days before your appointment.
If your address or phone number changes or if you need to change or cancel your appointment please telephone the appropriate phone numbers below during business hours:
Specialised endocrine clinics on Tel: 9382 4602
Specialised diabetes clinics on Tel: 9382 4600
Please bring
- Recent blood test results. If you do not have a copy of your results, please bring the name of the pathology company that performed the test so we can follow up with them.
- Any scans and reports related to your hormone condition.
- A list of all the medicines you are currently taking including any herbal or over the counter medicines.
When you come to our hospital for your appointment, you can check-in using our electronic check-in kiosks. These are located in our Adult Outpatient Department, Acute Services Building (Botany Street), High Street and Barker Street entrances.

Please let us know if you need an interpreter before your appointment date. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and call:
Specialised endocrine clinics on Tel: 9382 4602
Specialised diabetes clinics on Tel: 9382 4600
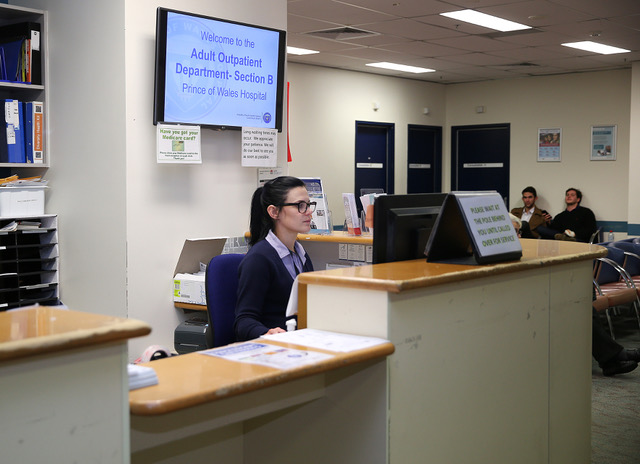
Outpatients Department
How we can help you
The Adult Outpatient Department provides outpatient appointments with doctors, nurses, and allied health professionals from a range of surgical and medical specialties. Most outpatient appointments are managed through this Department, however, some specialties manage their own appointments and have different locations within Prince of Wales.
We provide outpatient clinics across a range of surgical and medical specialties, including:
- Aged care
- Cardiology - Pacemaker
- Cognitive disorders
- Colorectal
- Dermatology
- Endocrinology
- ENT
- Fracture
- Gastroenterology
- General surgery
- Infectious diseases
- Immunology
- Neurointervention and Neurovascular
- Neurosurgery
- Orthopaedics
- Palliative and Supportive Care MDC
- Prescription and Opioid Pain management
- Plastic and reconstructive surgery
- Rheumatology
- Spinal injuries
Department Opening hours
8.00am - 5.30pm, Monday to Friday
Closed weekends and public holidays
Phone Operating Hours
8:30am – 4:30pm, Monday to Friday
Closed weekends and public holidays
How to find us
Level 2 , Campus Centre, Prince of Wales Hospital (Building 16 on our campus map)
Information about how to get to our Randwick campus
We are a team of different health professionals including Doctors, Nurses, Allied Health and Administration officers.
You will need a referral letter from your local general practitioner (GP) or specialty doctor to use this service. Your doctor will need to submit this referral electronically via Healthlink. Your referral will include your medical history, relevant test results, X-ray results and what medicines you are currently taking.
Once we receive this referral and accept it we will send you a letter with your appointment details. We will also send this to your doctor. If we cannot make an appointment for you, we will send you a letter confirming that you are on the waiting list for the next available appointment.
If you provide your mobile phone number you will receive a SMS reminder in the week before your appointment.
If your address or phone number changes or if you need to change or cancel your appointment please telephone 02 9382 0400.
Can I chose the day and time I attend the department for my appointment?
We have doctor clinics, allied health clinics and nursing clinics at set times. We try to find an appointment time that allows you to attend.
Will I always see the same doctor at each visit?
The Prince of Wales Hospital is a teaching hospital so you will be seen by a specialist doctor or a specialist doctor in training. You will stay under the care of the specialist doctor but you may see the doctor in training for your appointments.
What should I bring to my appointment?
- Current Medicare card or Veteran Affairs card
- Any Health Care Card, Pensioner Concession Card, or Commonwealth Seniors Health Care Card.
- Insurer details (eg workers compensation, public liability or third party).
- Recent X-rays or medical images and their reports, if applicable.
- Activities to keep you entertained while waiting (for example, a book, music player with headphones, crosswords). There are televisions in the waiting area.
- If you have any particular medical needs, we suggest you come prepared (for example, bring your medicines, if you are a diabetic, please bring food).
- To avoid missing your appointment we suggest you collect refreshments from the cafes located in the foyer of the hospital before checking in. If you need to leave the waiting area for any reason, please inform staff at the reception desk.
Who can I bring with me to my appointment?
We have limited seating in our waiting areas, we recommend bringing only one support person (for example, a family member, friend, or carer) with you.
Can I eat and take my medicines before my appointment?
You can eat and take medicines as normal unless the doctor has told you to stop taking medicines or not to eat. It is a good idea to bring any medicines you may need to take during the time you are at your appointment.
Waiting times for an appointment will vary for each speciality and is dependent on the seriousness of individual medical conditions. The department is busy and there may be delays. Most people are seen within 1 to 3 hours. We ask that you arrive at your allocated appointment time.
Appointment Reminders
If we have your mobile phone number, you will receive a text message reminding you of your appointment date and time 3 days before your appointment.
Please let us know if you need an interpreter before the date of your appointment. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak, and then ask the interpreter to set up a telephone conversation between you, an interpreter, and us on 9382 0400.
When you come to our hospital for your appointment, you can check-in using our electronic check-in kiosks. These are located in our Adult Outpatient Department, Acute Services Building (Botany Street), High Street and Barker Street entrances.

We are a teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
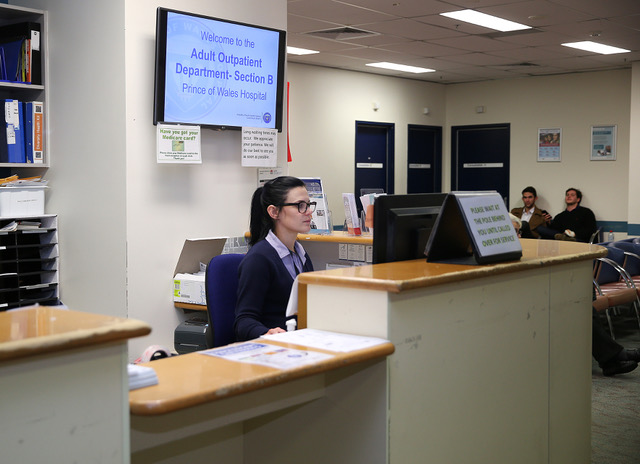
Outpatients Department
How we can help you
The Adult Outpatient Department provides outpatient appointments with doctors, nurses, and allied health professionals from a range of surgical and medical specialties. Most outpatient appointments are managed through this Department, however, some specialties manage their own appointments and have different locations within Prince of Wales.
We provide outpatient clinics across a range of surgical and medical specialties, including:
- Aged care
- Cardiology - Pacemaker
- Cognitive disorders
- Colorectal
- Dermatology
- Endocrinology
- ENT
- Fracture
- Gastroenterology
- General surgery
- Infectious diseases
- Immunology
- Neurointervention and Neurovascular
- Neurosurgery
- Orthopaedics
- Palliative and Supportive Care MDC
- Prescription and Opioid Pain management
- Plastic and reconstructive surgery
- Rheumatology
- Spinal injuries
Department Opening hours
8.00am - 5.30pm, Monday to Friday
Closed weekends and public holidays
Phone Operating Hours
8:30am – 4:30pm, Monday to Friday
Closed weekends and public holidays
How to find us
Level 2 , Campus Centre, Prince of Wales Hospital (Building 16 on our campus map)
Information about how to get to our Randwick campus
We are a team of different health professionals including Doctors, Nurses, Allied Health and Administration officers.
You will need a referral letter from your local general practitioner (GP) or specialty doctor to use this service. Your doctor will need to submit this referral electronically via Healthlink. Your referral will include your medical history, relevant test results, X-ray results and what medicines you are currently taking.
Once we receive this referral and accept it we will send you a letter with your appointment details. We will also send this to your doctor. If we cannot make an appointment for you, we will send you a letter confirming that you are on the waiting list for the next available appointment.
If you provide your mobile phone number you will receive a SMS reminder in the week before your appointment.
If your address or phone number changes or if you need to change or cancel your appointment please telephone 02 9382 0400.
Can I chose the day and time I attend the department for my appointment?
We have doctor clinics, allied health clinics and nursing clinics at set times. We try to find an appointment time that allows you to attend.
Will I always see the same doctor at each visit?
The Prince of Wales Hospital is a teaching hospital so you will be seen by a specialist doctor or a specialist doctor in training. You will stay under the care of the specialist doctor but you may see the doctor in training for your appointments.
What should I bring to my appointment?
- Current Medicare card or Veteran Affairs card
- Any Health Care Card, Pensioner Concession Card, or Commonwealth Seniors Health Care Card.
- Insurer details (eg workers compensation, public liability or third party).
- Recent X-rays or medical images and their reports, if applicable.
- Activities to keep you entertained while waiting (for example, a book, music player with headphones, crosswords). There are televisions in the waiting area.
- If you have any particular medical needs, we suggest you come prepared (for example, bring your medicines, if you are a diabetic, please bring food).
- To avoid missing your appointment we suggest you collect refreshments from the cafes located in the foyer of the hospital before checking in. If you need to leave the waiting area for any reason, please inform staff at the reception desk.
Who can I bring with me to my appointment?
We have limited seating in our waiting areas, we recommend bringing only one support person (for example, a family member, friend, or carer) with you.
Can I eat and take my medicines before my appointment?
You can eat and take medicines as normal unless the doctor has told you to stop taking medicines or not to eat. It is a good idea to bring any medicines you may need to take during the time you are at your appointment.
Waiting times for an appointment will vary for each speciality and is dependent on the seriousness of individual medical conditions. The department is busy and there may be delays. Most people are seen within 1 to 3 hours. We ask that you arrive at your allocated appointment time.
Appointment Reminders
If we have your mobile phone number, you will receive a text message reminding you of your appointment date and time 3 days before your appointment.
Please let us know if you need an interpreter before the date of your appointment. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak, and then ask the interpreter to set up a telephone conversation between you, an interpreter, and us on 9382 0400.
When you come to our hospital for your appointment, you can check-in using our electronic check-in kiosks. These are located in our Adult Outpatient Department, Acute Services Building (Botany Street), High Street and Barker Street entrances.

We are a teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
Respiratory and Sleep Medicine Department and Chest Clinic
How we can help you
We diagnose and support people with respiratory and sleep problems.
Reception
Phone: 02 9382 4643 or 9382 4631
Sleep Unit
Phone: 02 9382 8484
Lung Function Lab
Phone: 02 9382 4632
Opening times
8.00am - 5.00pm, Monday to Friday
Closed on weekends and public holidays.
How to find us
Level 2, Dickinson Building (Building 15 on our campus map)
Information about how to get to our Randwick campus
Respiratory and Sleep Consultants or doctors in training who assess, treat and help you to manage your respiratory and/or sleep problems.
A team of nurses who specialise in tuberculosis education and screening.
Lung function laboratory staff, hospital scientists that perform lung function tests and other diagnostic tests.
Sleep technicians book and supervise sleep studies, provide education sessions on operating your breathing machine, download data, perform mask fittings and can help you if you have problems with your machine.
Health education officer offers counselling for smoking cessation, asthma education and also manages our clinical research trials.
Administration staff will help you make appointments, inform you about what will happen at the Respiratory and Sleep Department and help to answer any questions you may have about your appointment.
We work in partnership with your local family doctor (GP) and Pulmonary Rehabilitation programs.
Clinic |
Attending Specialist |
Description of Clinic |
Respiratory and sleep clinicMonday 12.15pm |
Dr Elizabeth Brown, Respiratory and sleep physician |
Special interests in cystic fibrosis and obstructive sleep apnoea (OSA) research including recruitment for a multicentre trial of mandibular advancement splint and other trials of novel treatments for OSA. |
Respiratory and sleep disorders clinicTuesday 9.00am |
Dr Chaminda Lewis, Respiratory and sleep physician |
Clinic includes both general respiratory and sleep with a special focus on non-invasive ventilation (NIV), spinal cord injury and neuromuscular diseases. Special interests in interstitial lung disease (ILD), pleural disease, endobronchial ultrasound (EBUS), sleep medicine, NIV in complex patients with spinal injuries and neuromuscular disorders. |
Tuberculosis clinic (Chest)Wednesday 9.00am |
Dr Con Zois |
Services include diagnosing and managing active TB, screening for latent TB infection (LTBI) among health care workers, those exposed to TB, migrants and the immune suppressed and treating LTBI, organising radiology surveillance as well as BCG vaccination service. A referral is needed from the nurse’s clinic. |
Respiratory and sleep clinicThursday 8.30am |
Dr Emily Kemp |
Professor Thomas has a particular interest in sarcoidosis. He also sees patients with other immunological diseases of the lung, severe asthma, COPD and lung cancer. He is also an international expert on diving medicine. |
Respiratory and sleep clinicThursday 1.00pm |
Dr Nicholas Murray, Respiratory and sleep Physician, Head of Department |
General respiratory and sleep medicine, interventional pneumonology including endobronchial ultrasound (EBUS), interstitial lung disease, neuromuscular disease, cystic fibrosis and diving medicine. |
Respiratory and sleep clinicFriday 9.00am |
Dr Paul Lilburn, Interventional Pulmonologist | Clinic includes both general respiratory and sleep medicine patients, however with a specific interest in patients requiring specialist bronchoscopic interventions for advanced lung diseases or lung cancer. |
Lung function laboratoryMonday to Friday 9.00am - 5.00pm |
Lung function laboratory staff |
Offers a range of lung function and exercise tests for both inpatients and outpatients. This includes; skin allergy testing, investigation for home oxygen, fitness to fly tests and saline challenge tests used for diagnosing asthma and suitability for scuba diving. |
Nurses clinicMonday, Wednesday, Friday 8.30am |
Nurses |
Our nurses clinic provides TB screening (TST/Mantoux), including screening for immigration, TB education and BCG vaccinations. |
Sleep laboratoryMonday to Friday 9.00am - 5.00pm, plus overnight stays |
Sleep laboratory staff |
|
Bronchoscopy serviceTuesday, Thursday & Friday 8.30am |
Respiratory staff specialists | Performs standard flexible and rigid bronchoscopy, linear (convex probe) and radial mini-probe endobronchochial ultrasound (EBUS), pleural procedures for both inpatients and outpatients including thoracocentesis, intercostal catheter insertion and tunnelled "in dwelling" pleural catheters eg. PleuraX catheters. Advanced bronchoscopic procedures such as central airway recanalisation through mechanical rigid bronchoscopy, diathermy, Argon Plasma Coagulation (APC), Cryotherapy and Cyrosection, Snare electrocautery, airway stent insertion, transbronchical cryobiopsy, and medstinal lymph node cyrobiopsy. These procedures usually require referral from a Respiratory specialist. |
Smoking cessationAsthma educationMonday - Thursday 9.00am -5.00pm |
Provides individual counselling service to help patients and staff to quit smoking. Offers outpatient asthma education. |
To attend one of our clinics you will need a referral letter from your local general practitioner (GP) explaining your medical history, relevant test results, X-ray results and what medicines you are currently taking. Your GP can refer you directly for a home sleep study by providing a STOP BANG and Epworth Sleepiness Score in your referral.
Ask your GP to complete this referral electronically via Healthlink. See this webpage for further information around electronic referrals.
Once we have received your referral, we will send you and your GP a letter with appointment details. If we cannot make an appointment for you, we will send you a letter confirming that you are on the outpatient waiting list for the next available appointment.
If you need to change or cancel your appointment or no longer require an appointment, please contact 02 9382 4631 or 02 9382 4643.
- Our medical clinics and lung function clinics are covered by Medicare.
- There is no charge for our weekly TB clinic.
- Tuberculosis screening for health care workers and students carries a fee of $75.00 payable at our cashier’s office.
Yes, we are always looking for patients who would be happy to participate in clinical trials. These often asses the effectiveness of new medication for asthma and Chronic obstructive pulmonary disease (COPD). To find out more please contact us.
Doctor clinics
You may need to wait up to 9-12 months before you can see a Respiratory Consultant.
It is a busy centre and there could be delays when you arrive for your clinic appointment. Most people are seen within one to three hours.
Nurses Clinic
The waiting period for the nurse’s clinic is usually between 1 and 3 weeks.
Lung Function Clinic
The waiting period for the Lung Function clinic is usually between 1 and 3 weeks, but depends on the test you need. If you need a test urgently we usually will organise this to happen within a few days.
It is a busy department and there could be delays when you arrive for your clinic appointment. Most people are seen within one to three hours. We ask that you arrive at your scheduled appointment time to prevent waiting even longer.
You will see a nurse who will measure your weight, height, blood pressure, pulse and temperature.
You may also see a hospital scientist who may perform lung function testing.
- Your Medicare card
- Any relevant recent test results
- You are welcome to bring a support person (a relative, friend or carer) with you.
Please let us know if you need an interpreter before your appointment. You can contact us phoning the Translating and Interpreting Service (TIS) National on 131 450. Tell the operator what language you speak, and then ask the interpreter to set up a telephone conversation between you, an interpreter, and our service.
We are teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
Respiratory and Sleep Medicine Department and Chest Clinic
How we can help you
We diagnose and support people with respiratory and sleep problems.
Reception
Phone: 02 9382 4643 or 9382 4631
Sleep Unit
Phone: 02 9382 8484
Lung Function Lab
Phone: 02 9382 4632
Opening times
8.00am - 5.00pm, Monday to Friday
Closed on weekends and public holidays.
How to find us
Level 2, Dickinson Building (Building 15 on our campus map)
Information about how to get to our Randwick campus
Respiratory and Sleep Consultants or doctors in training who assess, treat and help you to manage your respiratory and/or sleep problems.
A team of nurses who specialise in tuberculosis education and screening.
Lung function laboratory staff, hospital scientists that perform lung function tests and other diagnostic tests.
Sleep technicians book and supervise sleep studies, provide education sessions on operating your breathing machine, download data, perform mask fittings and can help you if you have problems with your machine.
Health education officer offers counselling for smoking cessation, asthma education and also manages our clinical research trials.
Administration staff will help you make appointments, inform you about what will happen at the Respiratory and Sleep Department and help to answer any questions you may have about your appointment.
We work in partnership with your local family doctor (GP) and Pulmonary Rehabilitation programs.
Clinic |
Attending Specialist |
Description of Clinic |
Respiratory and sleep clinicMonday 12.15pm |
Dr Elizabeth Brown, Respiratory and sleep physician |
Special interests in cystic fibrosis and obstructive sleep apnoea (OSA) research including recruitment for a multicentre trial of mandibular advancement splint and other trials of novel treatments for OSA. |
Respiratory and sleep disorders clinicTuesday 9.00am |
Dr Chaminda Lewis, Respiratory and sleep physician |
Clinic includes both general respiratory and sleep with a special focus on non-invasive ventilation (NIV), spinal cord injury and neuromuscular diseases. Special interests in interstitial lung disease (ILD), pleural disease, endobronchial ultrasound (EBUS), sleep medicine, NIV in complex patients with spinal injuries and neuromuscular disorders. |
Tuberculosis clinic (Chest)Wednesday 9.00am |
Dr Con Zois |
Services include diagnosing and managing active TB, screening for latent TB infection (LTBI) among health care workers, those exposed to TB, migrants and the immune suppressed and treating LTBI, organising radiology surveillance as well as BCG vaccination service. A referral is needed from the nurse’s clinic. |
Respiratory and sleep clinicThursday 8.30am |
Dr Emily Kemp |
Professor Thomas has a particular interest in sarcoidosis. He also sees patients with other immunological diseases of the lung, severe asthma, COPD and lung cancer. He is also an international expert on diving medicine. |
Respiratory and sleep clinicThursday 1.00pm |
Dr Nicholas Murray, Respiratory and sleep Physician, Head of Department |
General respiratory and sleep medicine, interventional pneumonology including endobronchial ultrasound (EBUS), interstitial lung disease, neuromuscular disease, cystic fibrosis and diving medicine. |
Respiratory and sleep clinicFriday 9.00am |
Dr Paul Lilburn, Interventional Pulmonologist | Clinic includes both general respiratory and sleep medicine patients, however with a specific interest in patients requiring specialist bronchoscopic interventions for advanced lung diseases or lung cancer. |
Lung function laboratoryMonday to Friday 9.00am - 5.00pm |
Lung function laboratory staff |
Offers a range of lung function and exercise tests for both inpatients and outpatients. This includes; skin allergy testing, investigation for home oxygen, fitness to fly tests and saline challenge tests used for diagnosing asthma and suitability for scuba diving. |
Nurses clinicMonday, Wednesday, Friday 8.30am |
Nurses |
Our nurses clinic provides TB screening (TST/Mantoux), including screening for immigration, TB education and BCG vaccinations. |
Sleep laboratoryMonday to Friday 9.00am - 5.00pm, plus overnight stays |
Sleep laboratory staff |
|
Bronchoscopy serviceTuesday, Thursday & Friday 8.30am |
Respiratory staff specialists | Performs standard flexible and rigid bronchoscopy, linear (convex probe) and radial mini-probe endobronchochial ultrasound (EBUS), pleural procedures for both inpatients and outpatients including thoracocentesis, intercostal catheter insertion and tunnelled "in dwelling" pleural catheters eg. PleuraX catheters. Advanced bronchoscopic procedures such as central airway recanalisation through mechanical rigid bronchoscopy, diathermy, Argon Plasma Coagulation (APC), Cryotherapy and Cyrosection, Snare electrocautery, airway stent insertion, transbronchical cryobiopsy, and medstinal lymph node cyrobiopsy. These procedures usually require referral from a Respiratory specialist. |
Smoking cessationAsthma educationMonday - Thursday 9.00am -5.00pm |
Provides individual counselling service to help patients and staff to quit smoking. Offers outpatient asthma education. |
To attend one of our clinics you will need a referral letter from your local general practitioner (GP) explaining your medical history, relevant test results, X-ray results and what medicines you are currently taking. Your GP can refer you directly for a home sleep study by providing a STOP BANG and Epworth Sleepiness Score in your referral.
Ask your GP to complete this referral electronically via Healthlink. See this webpage for further information around electronic referrals.
Once we have received your referral, we will send you and your GP a letter with appointment details. If we cannot make an appointment for you, we will send you a letter confirming that you are on the outpatient waiting list for the next available appointment.
If you need to change or cancel your appointment or no longer require an appointment, please contact 02 9382 4631 or 02 9382 4643.
- Our medical clinics and lung function clinics are covered by Medicare.
- There is no charge for our weekly TB clinic.
- Tuberculosis screening for health care workers and students carries a fee of $75.00 payable at our cashier’s office.
Yes, we are always looking for patients who would be happy to participate in clinical trials. These often asses the effectiveness of new medication for asthma and Chronic obstructive pulmonary disease (COPD). To find out more please contact us.
Doctor clinics
You may need to wait up to 9-12 months before you can see a Respiratory Consultant.
It is a busy centre and there could be delays when you arrive for your clinic appointment. Most people are seen within one to three hours.
Nurses Clinic
The waiting period for the nurse’s clinic is usually between 1 and 3 weeks.
Lung Function Clinic
The waiting period for the Lung Function clinic is usually between 1 and 3 weeks, but depends on the test you need. If you need a test urgently we usually will organise this to happen within a few days.
It is a busy department and there could be delays when you arrive for your clinic appointment. Most people are seen within one to three hours. We ask that you arrive at your scheduled appointment time to prevent waiting even longer.
You will see a nurse who will measure your weight, height, blood pressure, pulse and temperature.
You may also see a hospital scientist who may perform lung function testing.
- Your Medicare card
- Any relevant recent test results
- You are welcome to bring a support person (a relative, friend or carer) with you.
Please let us know if you need an interpreter before your appointment. You can contact us phoning the Translating and Interpreting Service (TIS) National on 131 450. Tell the operator what language you speak, and then ask the interpreter to set up a telephone conversation between you, an interpreter, and our service.
We are teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.